Updated June 02, 2022
An Aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible. This form asks the medical office for the right to be able to write a prescription to their patient whilst having Aetna cover the cost as stated in the insurance policy (in reference to prescription costs). The form must be completed by the medical staff and submitted to Aetna in the proper state jurisdiction.
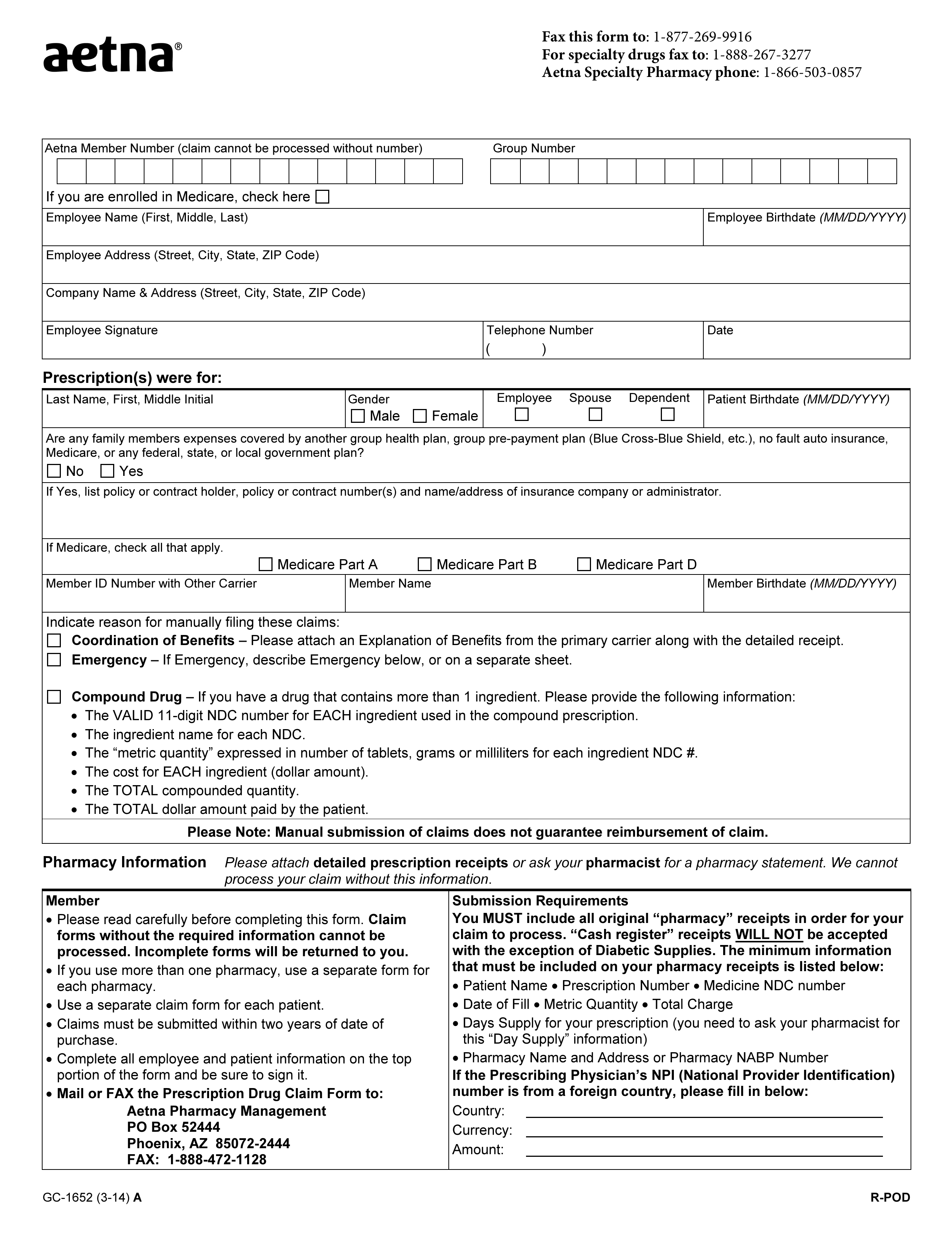
- Fax: 1 (877) 269-9916
- Fax (Specialty Drugs): 1 (888) 267-3277
- Aetna Specialty Pharmacy phone: 1 (866) 503-0857
- All Aetna Forms
By State
How to Write
Step 1 – Begin by providing the patient’s Aetna member number, group number, and specify whether or not the patient is enrolled in Medicare.
Step 2 – Provide the employee’s full name, date of birth, full address, company name, and company address. The employee must then supply their signature, telephone number, and date the signing.
Step 3 – In “Prescription(s) were for”, specify the patient’s full name, sex (m/f), indicate who the prescription is for, and provide the patient’s date of birth.
Step 4 – In “Prescription(s) were for”, select yes or no to indicate whether or not the patient’s family members’ expenses are covered by another group health plan, group pre-payment plan (Blue Cross, Blue Shield, etc.), no fault auto insurance, Medicare, or any federal, state, or local government plan. If yes, list the policy or contract holder, policy or contract number(s), and name/address of insurance company or administrator.
Step 5 – In “Prescription(s) were for”, specify the patient’s Medicare type. Also, provide the member ID number with other carrier along with the member’s name and birthdate.
Step 6 – In “Prescription(s) were for”, indicate the reason for manually filling the request.
Step 7 – In “Submission Requirements”, if the prescribing physician’s NPI number is from a foreign country, specify the physician’s country, currency, and amount.