Updated June 02, 2022
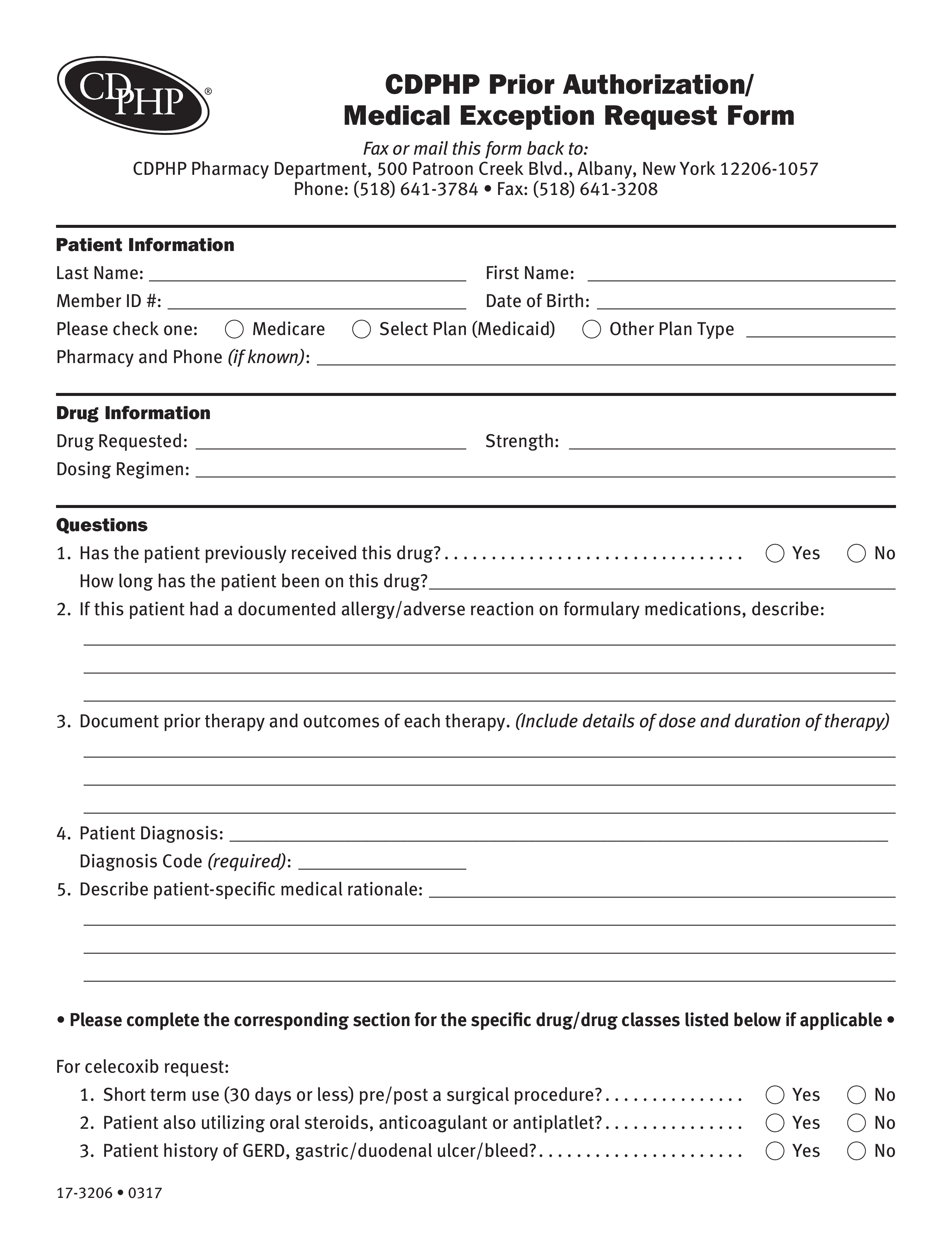
A CDPHP prior authorization form is a document that physicians will need to complete and submit in order to request coverage for an individual’s prescription. The form contains important information pertinent to the desired medication; CDPHP will analyze this information to discern whether or not a plan member’s diagnosis and requested medication is covered in the member’s health insurance plan. Have the form completed correctly before sending it by mail or fax to the appropriate address below.
- Fax: 1 (518) 641-3208
- Mail: CDPHP Pharmacy Department, 500 Patroon Creek Blvd., Albany, New York 12206-1057
- Phone: 1 (518) 641-3784
How to Write
Step 1 – In “Patient Information”, provide the patient’s full name, member ID number, and date of birth. Select one of the available options to specify the patient’s plan type (if other, explain). Also, give the pharmacy name and phone number (if available).
Step 2 – In “Drug Information”, specify the drug being requested, dose, and dosing regimen.
Step 3 – In “Questions (1)”, select yes or no as to whether or not the patient has previously received this medication (if yes, indicate how long the patient has been on this medication).
Step 4 – In “Questions (2)”, explain any allergy/adverse reactions the patient is known to experience on formulary medications.
Step 5 – In “Questions (3)”, explain any prior therapy and the outcome(s) (include dose and duration).
Step 6 – In “Questions (4)”, specify the patient’s diagnosis and diagnosis code (if required).
Step 7 – In “Questions (5)”, describe any patient-specific rationale.
Step 8 – In “For celecoxib request”, select yes or no in response to the following questions:
- Short term use (30 days or less) pre/post a surgical procedure?
- Patient also utilizing oral steroids, anticoagulant or antiplatlet?
- Patient history of GERD, gastric/duodenal ulcer/bleed?
Step 9 – In “For a reproductive endocrinology drug request”, respond to the following:
- Treatment request is being used for such as timed intercourse or IUI
- Prior number of cycles medication used for
- Dates of prior treatments
- Outcome of prior treatments
Step 10 – In “For Xolair (omalizumab) request”, respond to the following:
- IgE level and date of test
- Does the patient currently use any tobacco products? (y/n)
- Allergic sensitivity including type of test conducted
Step 11 – In “For Procrit, Epogen or Aranesp”, respond to the following:
- Hemoglobin (Hgb) (g/dl) and date of test
- Hematocrit (Hct) (%) and date of test
- Ferritin (ng/ml) and date of test
- Transferrin saturation (TSAT) (%) and date of test
Step 12 – In “For weight management drug request”, specify the patient’s height, weight and date taken, comorbidities (hypertension, diabetes, hyperlipidemia, etc.), and diet and exercise history.
Step 13 – In “For Androgel or Androderm request”, specify the patient’s symptoms currently being treated and provide the dates and results of two early morning total testosterone levels (ng/dl).
Step 14 – In “Practitioner Information”, the practitioner must give their signature, name, phone number, EIN, address, NPI number, fax number, nurse contact with ext., and specify the date of the request.