Updated July 27, 2023
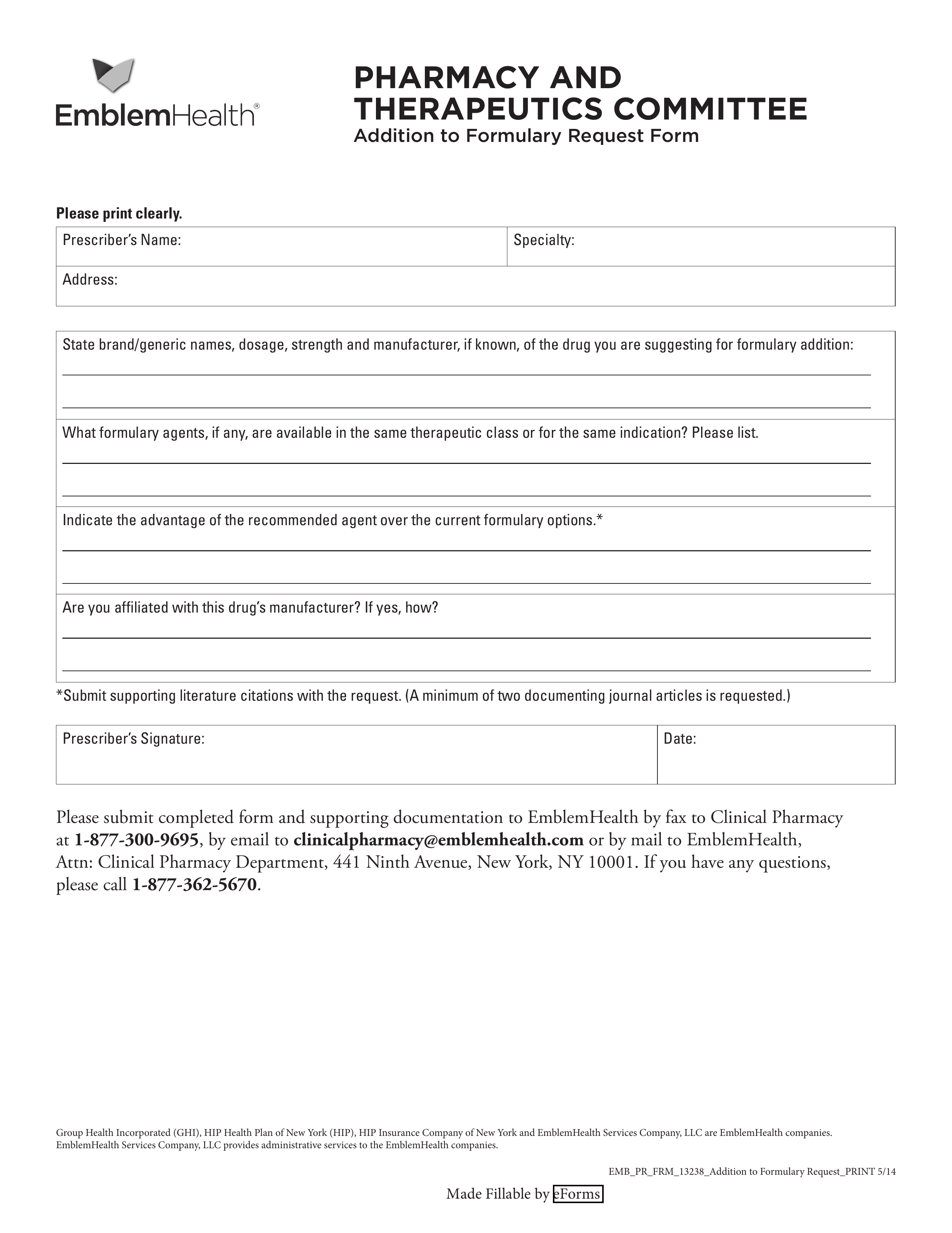
An EmblemHealth prior authorization form is a document used when requesting medical coverage from an individual’s health plan, specifically for prescription drugs. This form may be filled out by the enrollee, the prescriber, or an individual requesting coverage on the enrollee’s behalf.
- Fax: 1 (877) 300-9695
- Email: clinicalpharmacy@emblemhealth.com
- Mail: EmblemHealth, Attn: Clinical Pharmacy Department, 441 Ninth Avenue, New York, NY 10001
- Phone: 1 (877) 362-5670