Updated July 27, 2023
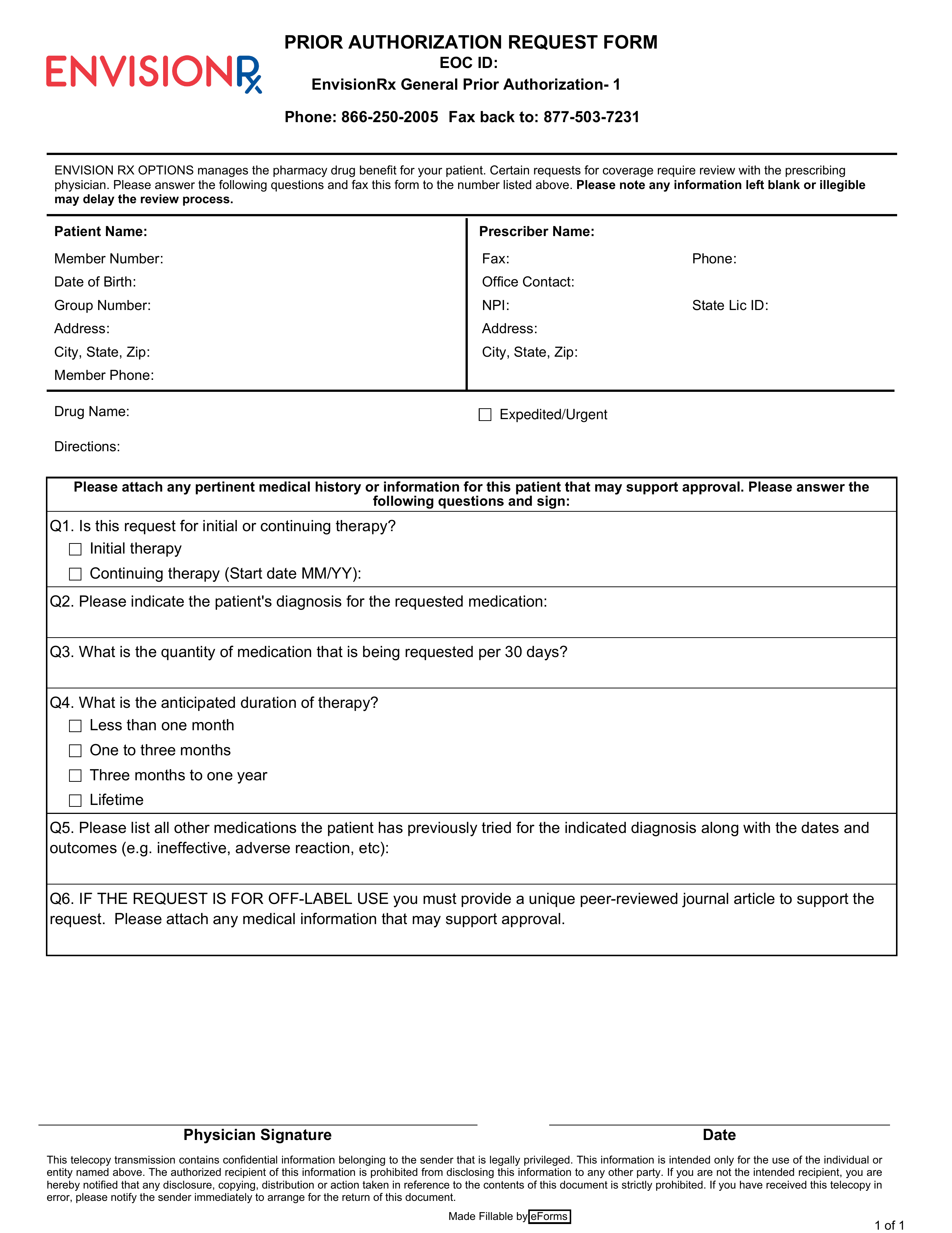
An EnvisionRx prior authorization form is a document used by a physician when seeking approval for a patient’s prescription. Once complete, the form will specify important details regarding the patient’s diagnosis, which in turn will allow EnvisionRx to ascertain whether or not the patient’s insurance plan covers the prescription cost. Have the form completed in its entirety before sending it by fax to EnvisionRx.
- Fax: 1 (877) 503-7231
- Phone: 1 (866) 250-2005