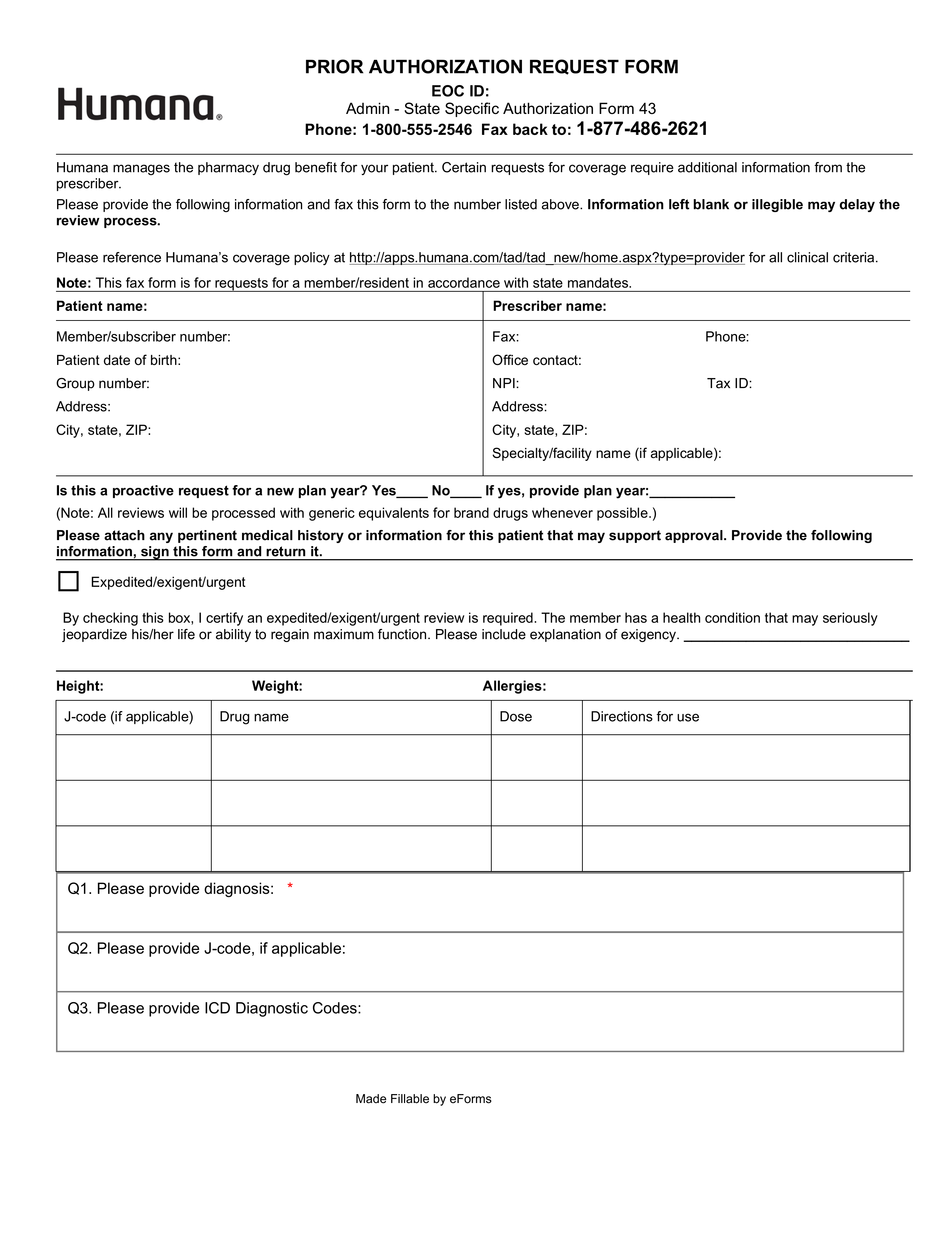
Updated July 27, 2023
A Humana Prior Authorization Form is filled out by a pharmacist in order to help a patient secure coverage for a certain medication. By submitting this form, the pharmacist may be able to have the medication covered by Humana. In your form, you will need to explain your rationale for making this request, including a clinical justification and referencing any relevant lab test results.
- Fax: 1 (800) 555-2546
- Phone: 1 (877) 486-2621
- Humana Universal Prior Authorization Form