Updated July 27, 2023
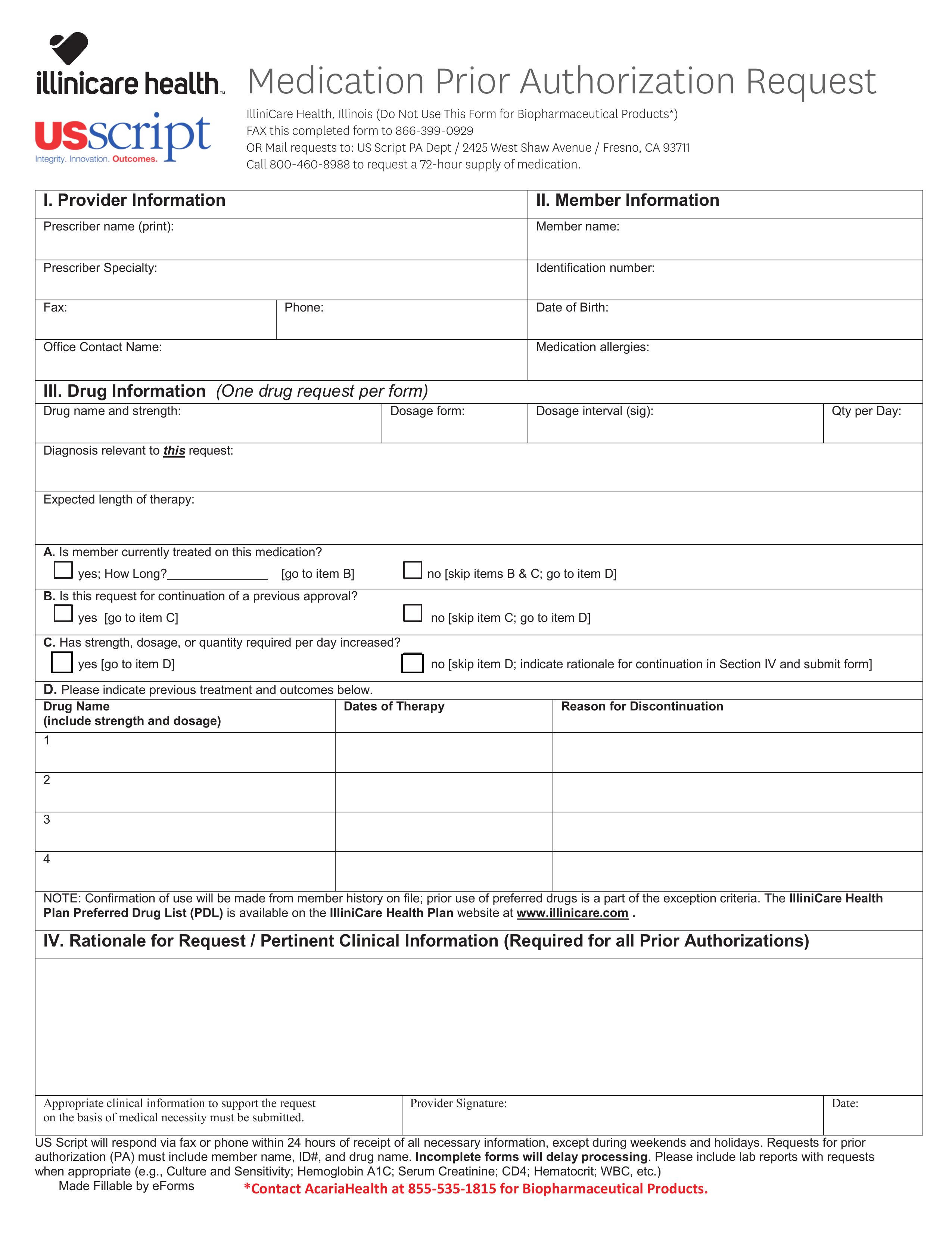
An Illinicare Health Prior Authorization Form allows a prescriber to request coverage for a proposed medication to the patient’s medical insurance provider. If your patient is a member of Illinicaire Health, you will be required to submit the Illinicare Health Prior Authorization Form which you can find attached to this webpage.
- Fax: 1 (866) 399-0929
- Phone: 1 (866) 329-4701