Updated July 27, 2023
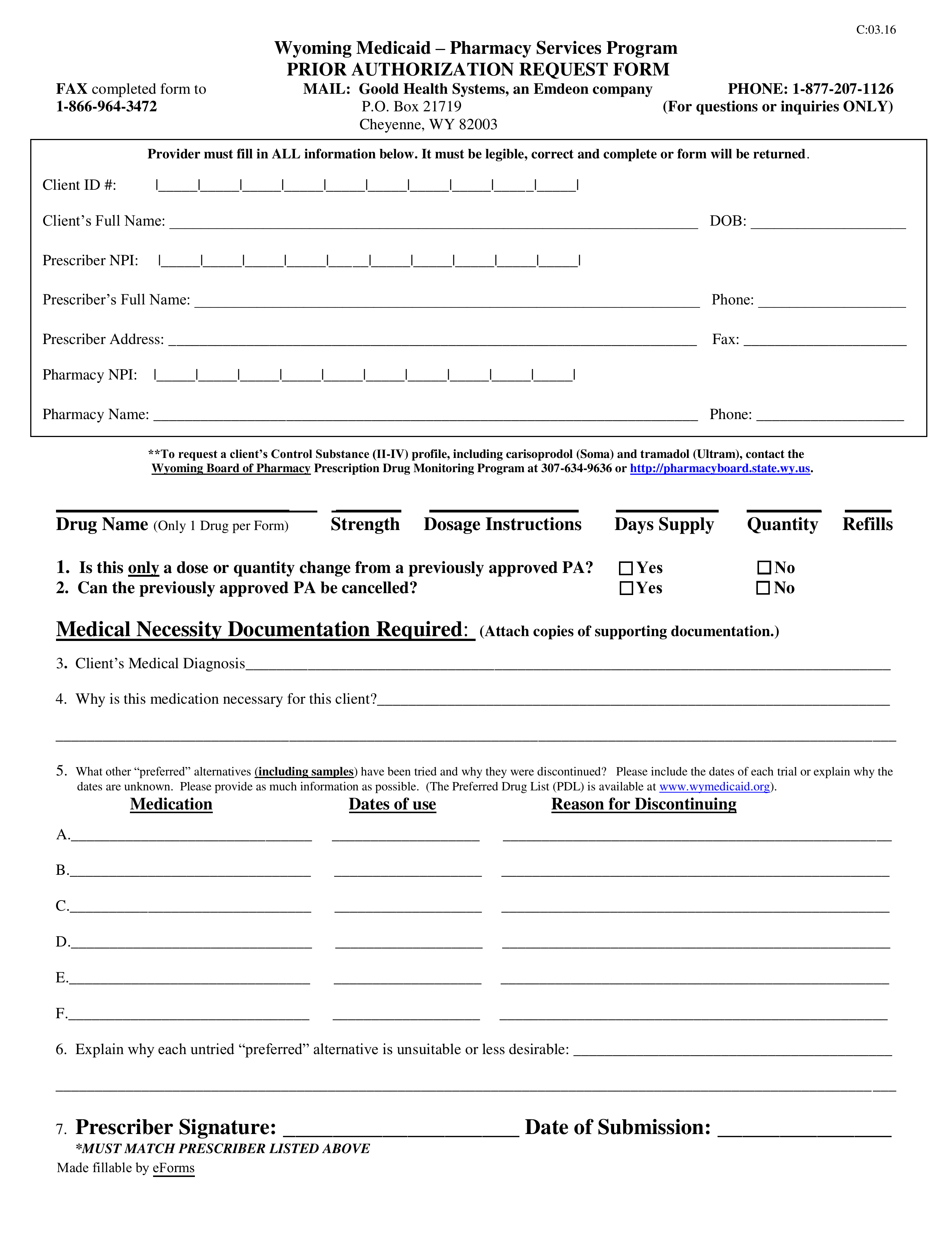
A Wyoming Medicaid prior authorization form is completed by a physician who wishes to prescribe a drug that is not on the preferred drug list (PDL) and submitted to the Wyoming Drug Utilization Review Board. When treating a patient, Medicaid providers in Wyoming are encouraged to prescribe medication found on the Wyoming Department of Health’s PDL. Once submitted, the request will be evaluated by the board and will only be approved if they deem it medically necessary. It’s up to the prescribing physician to rationalize their decision by providing medical reasoning for their choice of medication. Any documents that support their explanation should be attached to the request form. If the request is denied, the patient may choose to pay for this medication out of pocket or appeal the prior authorization.
Form can be faxed to: 1 (866) 964-3472
Phone number: 1 (877) 207-1126