Updated November 27, 2023
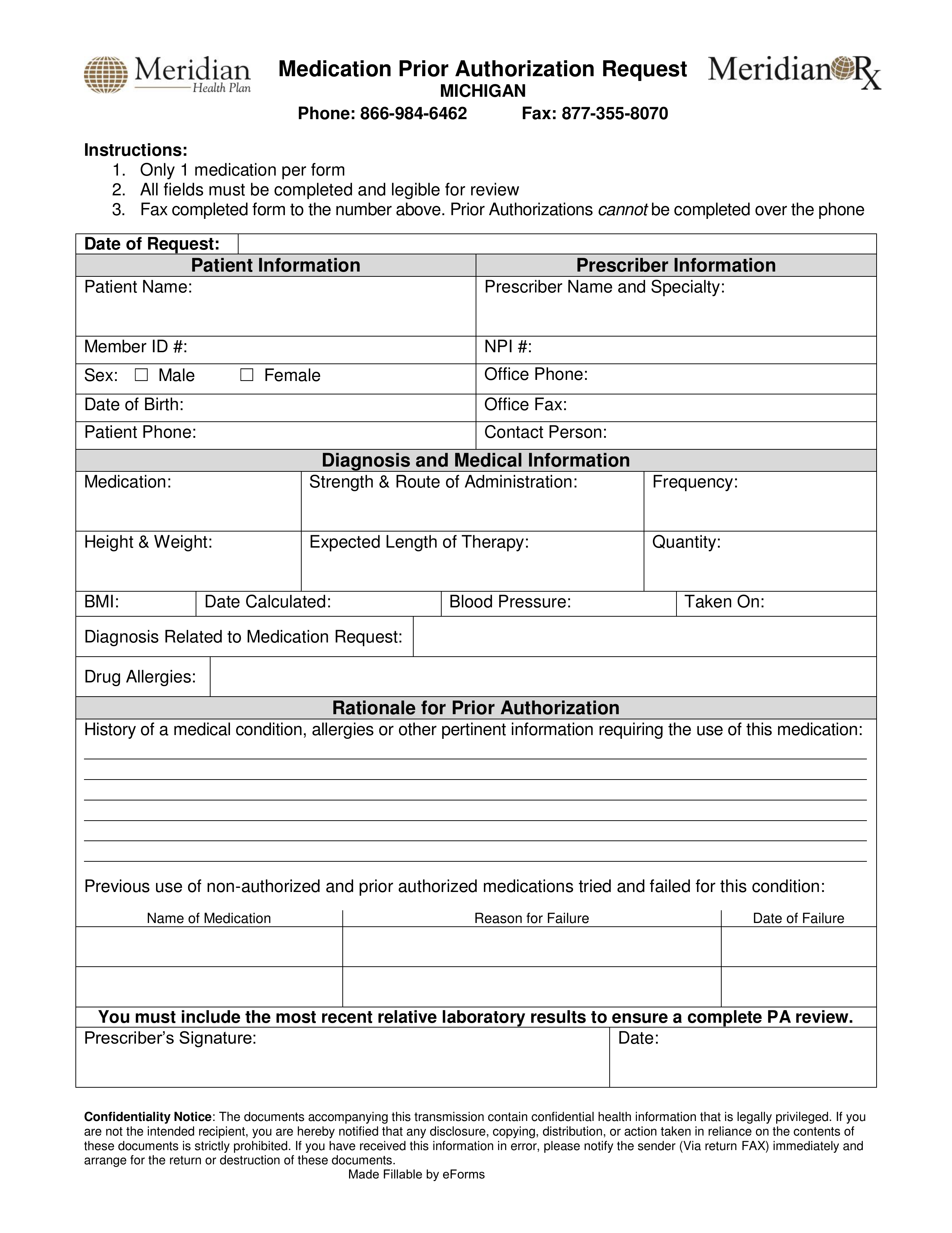
A Meridian prior authorization form is made for medical offices to fill out when requesting coverage for a non-preferred drug. A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been completed and submitted for review. Meridian has also provided an online prior authorization form for all interested parties.
- Fax (Michigan): 1 (877) 355-8070
- Fax (Illinois): 1 (855) 580-1695
- Phone: 1 (866) 984-6462
- Submit an Online Form
- All Meridian Forms