Updated July 27, 2023
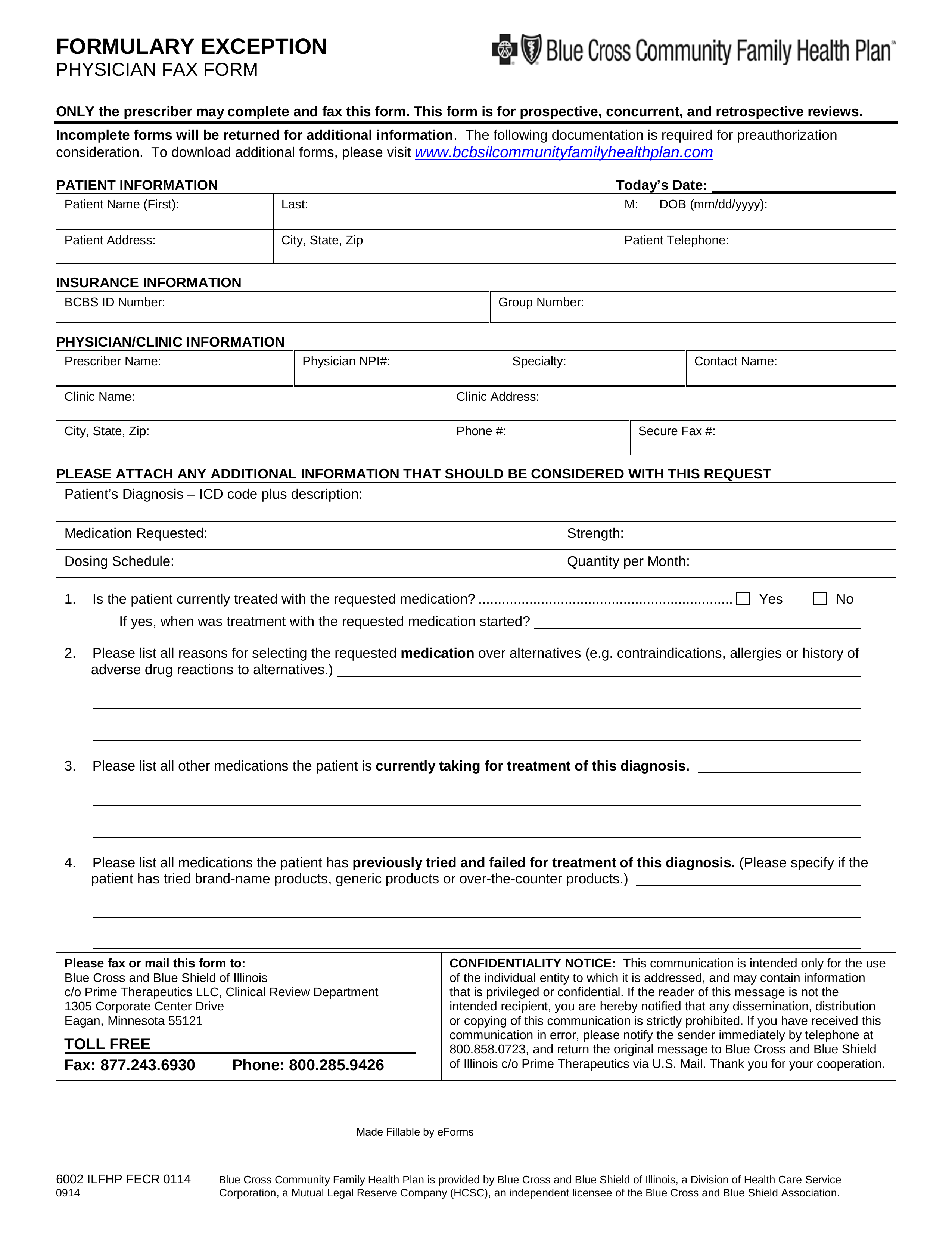
A Prime Therapeutics prior authorization form, also known as a Formulary Exception Form, is used to request coverage for a patient’s prescription that isn’t listed on their health insurance provider’s formulary. This document will contain the diagnosis and an explanation for why the prescription is suggested above those which are potentially more commonly used. On this page, you will find a fillable PDF version of this form which you can download, as well as the fax number that you must send it to.
- Prior Authorization Form
- Fax to: 1 (877) 243-6930
- Phone: 1 (800) 285-9426
- Part D Prior Authorization Form (Medicare)
- Part D Fax to: 1 (800) 693-6703