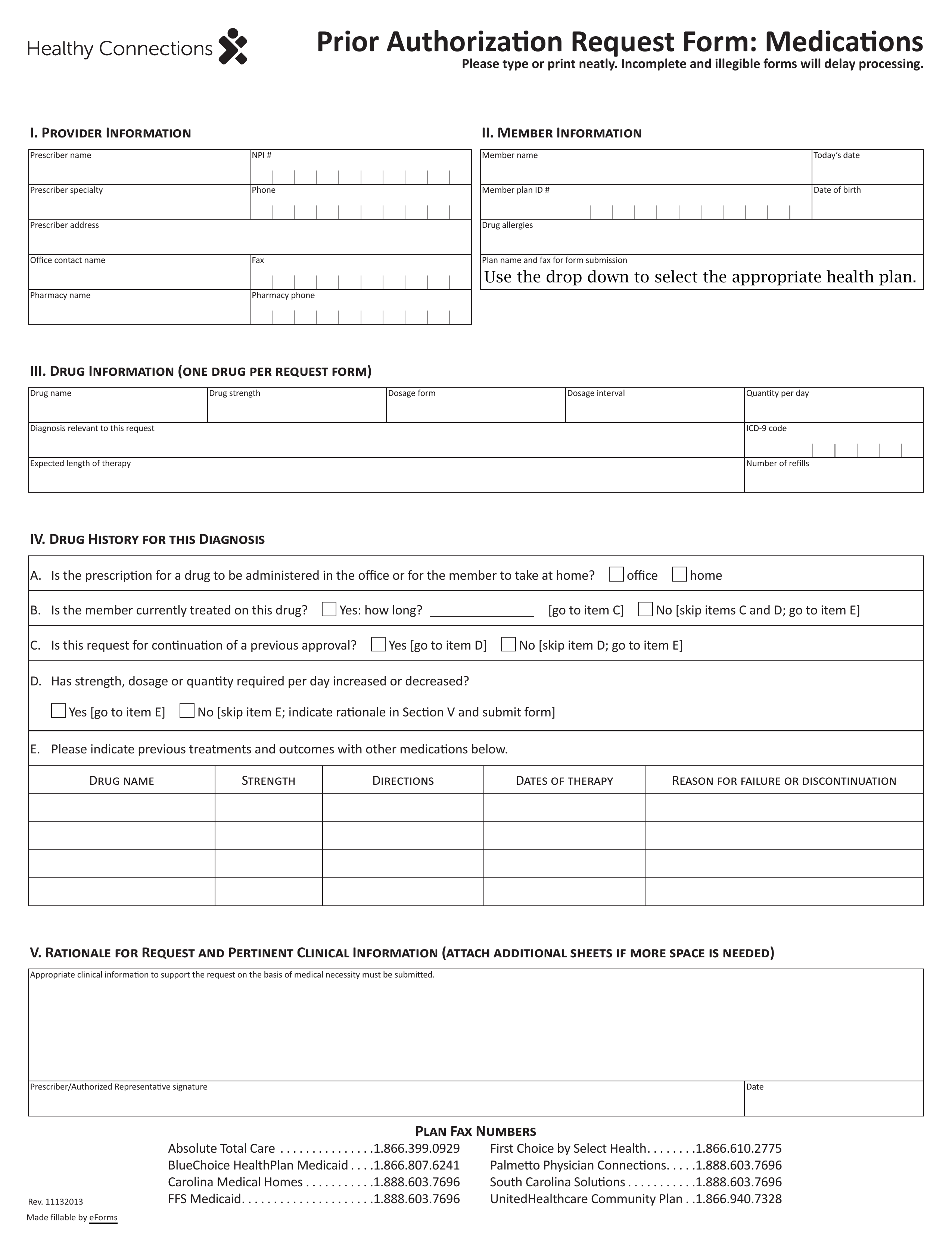
Updated July 27, 2023
A SelectHealth prior authorization form is a form used by a physician to request a specific medication/treatment for their patient, one that is otherwise not covered by the patient’s insurance plan. SelectHealth needs to make sure that the doctor has considered other options for treating their patient and that this particular treatment is the only viable option to improve their patient’s condition. Upon completion of the SelectHealth prior authorization form, the physician can fax or mail it to SelectHealth so that the insurance company can determine whether to sanction this request. Physician’s should include as much information concerning their diagnoses and medical reasoning as possible in order to establish a sound argument.
- Form can be faxed to: 1 (866) 610-2775