Updated June 02, 2022
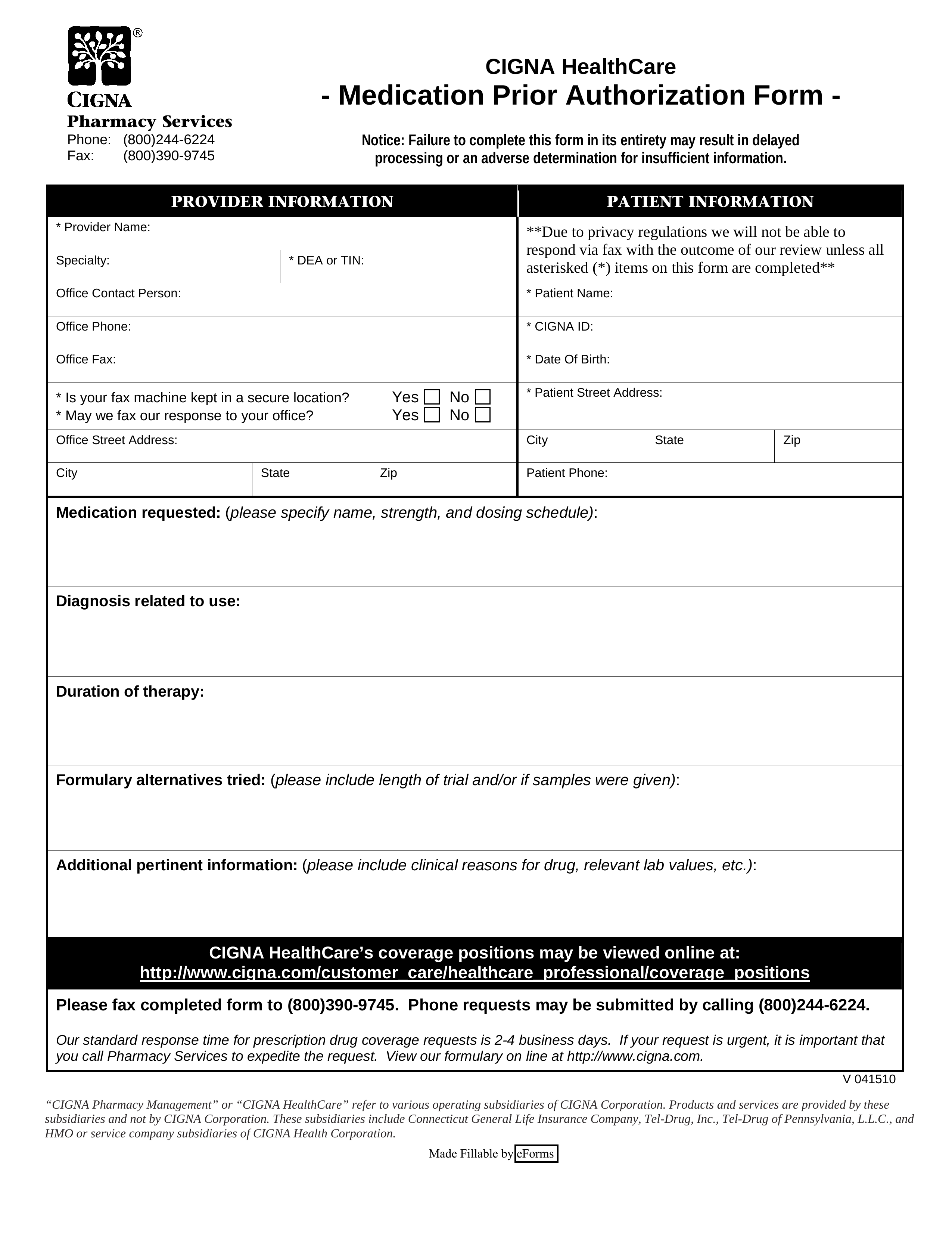
A Cigna prior authorization form is required for Cigna to cover the cost of certain prescriptions for clients they insure. Cigna will use this form to analyze an individual’s diagnosis and ensure that their requested prescription meets eligibility for medical coverage. This particular form can be submitted by phone as well as fax (contact numbers available below).
- Fax: 1 (800) 390-9745
- Phone: 1 (800) 244-6244
How to Write
Step 1 – In “Provider Information”, specify the provider’s name, specialty, and DEA or TIN. Also, provide an office contact name, office phone number, and office fax number.
Step 2 – In “Provider Information”, specify whether or not the medical office’s fax machine is in a secure location, and whether or not Cigna can fax their response to said medical office.
Step 3 – In “Patient Information”, provide the patient’s ID number, Cigna ID number, date of birth, full address, and phone number.
Step 4 – In “Medication requested”, specify the medication name, strength, and dosing schedule.
Step 5 – In “Diagnosis related to use”, explain the patient’s diagnosis which requires the prescription.
Step 6 – In “Duration of therapy”, specify for how long the patient will require said medication.
Step 7 – In “Formulary alternatives tried”, mention any other medications or therapies tried (include length of trial and/or if samples were given).
Step 8 – In “Additional pertinent information”, provide the clinical reasons for drug, relevant lab values, etc.