Updated April 05, 2024
An advance directive allows a patient to choose end-of-life treatment options and choose an agent to make medical decisions on their behalf. It only becomes in effect if the patient is no longer able to make decisions for themselves due to incapacity or impairment.
By State
- Alabama
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- Florida
- Georgia
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Carolina
- South Dakota
- Tennessee
- Texas
- Utah
- Vermont
- Virginia
- Washington
- Washington D.C.
- West Virginia
- Wisconsin
- Wyoming
Table of Contents |
What is an Advance Directive?
An advance directive allows a person (principal) to choose someone else (agent or proxy) to make health care decisions on their behalf and to create end-of-life treatment instructions. To complete, the form must be signed per state law, which often requires two witnesses or a notary public.
Once signed, the agent must present the advance directive to medical at each occurrence it is used.
What is Included? (4 parts)
- Medical Power of Attorney – An individual can assign an agent to make their medical decisions.
- Living Will – A written record with personal requests for inclusion and exclusion of certain medical treatments.
- Physician Orders for Life-Sustaining Treatment (POLST) – Detailed end-of-life options overviewed and recorded by a physician.
- Do Not Resuscitate Order (DNR) – Patients can opt in or out of life-sustaining measures, such as CPR.
What if the Principal is Already Incapacitated?
If the principal (the patient) is already incapacitated, the family will be required to obtain guardianship rights from the local court in order to make the patient’s medical decisions. In most circumstances, a hospital will allow the spouse or family member to act as the agent by default (although this may depend on local and state laws).
Advance Directive vs. Other Estate Forms
| Form | Healthcare Agent | Decide Treatments | Can Prohibit CPR |
|---|---|---|---|
| Advance Directive | √ | √ | √ |
| Medical Power of Attorney | √ | ||
| Living Will | √ | ||
| Do Not Resuscitate (DNR) | √ |
How to Get an Advance Directive (5 steps)
- Step 1 – Select an Agent
- Step 2 – Decide the Powers
- Step 3 – Choose End-of-Life Options
- Step 4 – Sign
- Step 5 – Register
Step 1 – Select an Agent

This is often referred to as the medical power of attorney portion that requires the principal to select an agent to represent their healthcare decisions. The agent may ONLY act if the principal cannot make decisions for themselves due to being incapacitated. The agent should understand the wishes of the principal and always keep their best interests in mind when making decisions.
- Second Agent – The principal is able to select a second agent to help in case the original agent is not able to perform. However, decision-making powers cannot be shared.
Step 2 – Decide the Powers

The principal will have to decide how much power to give the agent.
This mainly consists of:
- Electing to have the powers begin immediately or upon the principal’s incapacitation;
- Deciding to prolong the principal’s life as long as possible (even if there is no possible cure); and
- Selecting any post-death responsibilities (ordering an autopsy, where the remains are kept, etc.).
Any other powers should be mentioned to the agent verbally.
Step 3 – Choose End-of-Life Options

This is for the living will portion that allows the principal to select their plans if they should become in a vegetative state or uncurable situation. Under such an event, the principal can choose to stop any life support assistance such as halting breathing machines, food, or water intravenously (through an IV).
Do Not Resuscitate (DNR) – Used to inform medical personnel to not perform CPR or other life-saving procedures in the event that the principal’s heart stops beating or if they are not breathing.
Step 4 – Sign

Depending on the signing laws in your state, an advance directive must be signed with a notary public, two witnesses, or both. If given the choice, it’s recommended to have the document notarized.
A notary can be found online, at a local bank, or using a notary service.
Step 5 – Register

It’s best to store an advance directive in an easily accessible place in the event of an emergency. It’s common to record it with a state registry or a national organization. Wherever the advance directive is stored, the location should be recorded in a Wallet Card and kept on the principal at all times.
Signing Requirements
Where to Register an Advance Directive
An advance directive may be registered in either the principal’s state of residence or in a national registry (see below).
State Registries (Note: Not every state has a registry.)
- Alaska[1] – Donor Registry
- Arizona[2] – Online Registry
- California[3] – Registration Form
- Idaho[4] – Registration Form
- Louisiana[5] – Instructions
- Montana[6] – End-of-Life Registry
- Nevada – Registration Form
- North Carolina – Registration Form
- Vermont – Registration Form
- Virginia – Online Registration
- West Virginia[7] – Registration Form
- JoinCake – No fee
- U.S. Registry – $59.95 per five years ($25 for an additional five years)
- Everplans – $75 a year
Sample
Download: PDF, MS Word, OpenDocument
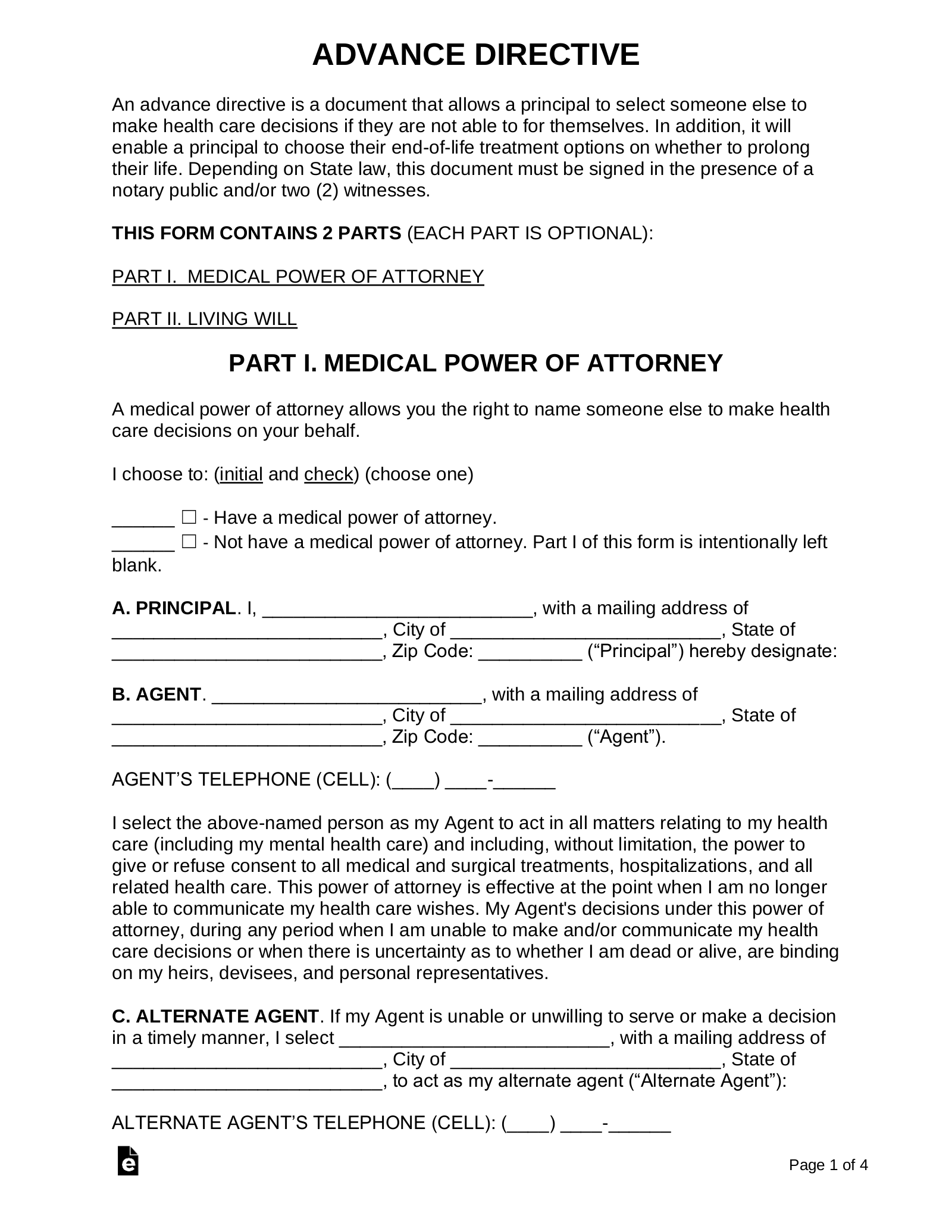
Advance Directive
PART I. MEDICAL POWER OF ATTORNEY
A medical power of attorney allows you the right to name someone else to make health care decisions on your behalf.
I choose to: (initial and check) (choose one)
[INITIALS] ☐ – Have a medical power of attorney.
[INITIALS] ☐ – Not have a medical power of attorney. Part I of this form is intentionally left blank.
A. PRINCIPAL. I, [NAME], with a mailing address of [ADDRESS], City of [CITY], State of [STATE], Zip Code: [ZIP] hereby designate:
B. AGENT. [NAME], with a mailing address of [ADDRESS], City of [CITY], State of [STATE], Zip Code: [ZIP]. AGENT’S TELEPHONE (CELL): [PHONE]
C. ALTERNATE AGENT. If my Agent is unable or unwilling to serve or make a decision in a timely manner, I select [NAME], with a mailing address of [ADDRESS], City of [CITY], State of [STATE], to act as my alternate agent. ALTERNATE AGENT’S TELEPHONE: [PHONE]
I intend for my Agent to receive any and all of my health records and information as if I were the one requesting such information.
PART II. LIVING WILL
A living will allows a principal to select end-of-life treatment options in the chance of incapacitation with no viable cure.
I choose to: (initial and check) (choose one)
- [INITIALS] ☐ – Have a living will.
- [INITIALS] ☐ – Not have a living will. Part II of this form is intentionally left blank.
A. PRINCIPAL. I, [NAME], with a mailing address of [ADDRESS], City of [CITY], County of [COUNTY], State of [STATE], with the last four (4) digits of my social security number (SSN) being [SSN] (“Principal”) desire to advise my doctors and medical providers of my wishes for my health care in the event I am not able to communicate my wishes.
B. LIFE SUPPORT.
I desire that my doctor make a concerted effort to return me to an acceptable quality of life using then available treatments and therapies. However, if my quality of life becomes unacceptable as I have defined below, and my doctors have determined that my condition will not improve (is irreversible), I direct that all treatments that extend my life be withdrawn.
An unacceptable quality of life means (initial and check all that apply):
- [INITIALS] ☐ – Chronic coma or persistent vegetative state
- [INITIALS] ☐ – No longer able to communicate my needs
- [INITIALS] ☐ – No longer able to recognize family or friends
- [INITIALS] ☐ – Total dependence on others for daily care
- [INITIALS] ☐ – Other: [DESCRIBE].
(initial and check) (choose one)
- [INITIALS] ☐ – Even if I have the quality of life described above, I still wish to be treated with food and water by tube or intravenously (IV).
- [INITIALS] ☐ – If I have the quality of life described above, I do NOT wish to be treated with food and water by tube or intravenously (IV).
C. CERTAIN LIFE-SUSTAINING TREATMENT.
Some people do not wish to have certain life-sustaining treatments under any circumstance, even if recovery is a possibility. Check the treatments below, if any, that you do not wish to have under any circumstances:
(initial and check) (choose one)
- [INITIALS] ☐ – Cardiopulmonary Resuscitation (CPR)
- [INITIALS] ☐ – Ventilation (breathing machine)
- [INITIALS] ☐ – Feeding tube
- [INITIALS] ☐ – Dialysis
- [INITIALS] ☐ – Other: [DETAILS].
D. END OF LIFE WISHES. (hospice care, funeral arrangements, etc.):
When I am near death, it is important to me that: [DETAILS]
I have signed this document on this [DAY] day of [MONTH], 20[YEAR].
Principal’s Signature: ___________________________________
Print Name: __________________________________
WITNESS 1
Signature: ___________________________________ Date: _______________
Print Name: __________________________________
WITNESS 2
Signature: ___________________________________ Date: _______________
Print Name: __________________________________