Updated February 12, 2024
A do-not-resuscitate (DNR) order is used for patients who do not want to be saved if their heart or breathing stops. This is generally the case for individuals with late stages of cancer or other advanced medical issues. The laws for withholding resuscitation are governed by each state and commonly include a requirement that the patient authorizes this form along with their primary care physician, notary public, or witness(es).
By State
- Alabama
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- Florida
- Georgia
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Carolina
- South Dakota
- Tennessee
- Texas
- Utah
- Vermont
- Virginia
- Washington
- Washington D.C.
- West Virginia
- Wisconsin
- Wyoming
Table of Contents |
What is a Do-Not-Resuscitate Order?
A do-not-resuscitate order, also referred to as a “DNR,” is for individuals who are terminally ill and do not want to be brought back to life via CPR, defibrillation, or other related options. This is common when a person is elderly or suffering from a health condition where there is no foreseeable path to a cured condition. To create a do-not-resuscitate order, in most states, the patient will need to have the form signed between themselves, their physician, and witnesses (if required).
How to Get a Do-Not-Resuscitate Order (4 steps)
- Speak with a Physician
- Decide on Future Medical Treatment
- Download, Complete, and Sign
- Store the Form in a Safe Place
1. Speak with a Physician
 A Do-Not-Resuscitate Order (DNR) is a medical directive to doctors and other first responders instructing them to withhold CPR treatment should a patient’s breathing or heart stop. Also called a “no code” or “allow natural death” order, the DNR is completed in conjunction with a physician, whose signature is required to implement it. The form may be completed in the hospital or elsewhere, but should be filed with other medical records so that all caregivers are made aware of this intention.
A Do-Not-Resuscitate Order (DNR) is a medical directive to doctors and other first responders instructing them to withhold CPR treatment should a patient’s breathing or heart stop. Also called a “no code” or “allow natural death” order, the DNR is completed in conjunction with a physician, whose signature is required to implement it. The form may be completed in the hospital or elsewhere, but should be filed with other medical records so that all caregivers are made aware of this intention.
Since filing a DNR is literally a matter of life and death, the document affirms that the patient is of “sound mind” – that the decision to refuse CPR has been made by the patient voluntarily and with a clear understanding of its implications.
2. Decide on Future Medical Treatment
 Contrary to common misconception, the DNR is not a blanket declaration covering all medical interventions. It relates only to cardiopulmonary resuscitation. Other modes of treatment, including the provision of drugs and chemotherapy, testing, and the vast array of supports in the modern medical arsenal are generally excluded.
Contrary to common misconception, the DNR is not a blanket declaration covering all medical interventions. It relates only to cardiopulmonary resuscitation. Other modes of treatment, including the provision of drugs and chemotherapy, testing, and the vast array of supports in the modern medical arsenal are generally excluded.
A DNR should be part of a more comprehensive plan for medical care. Patients generally have the right to choose which treatments to accept, but things can get more complicated if the patient is incapacitated or is otherwise unable to communicate with medical staff or family members. The best course is to formalize these more comprehensive care directives in a living will or advanced directive.
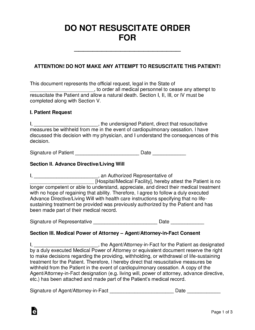
3. Download, Complete, and Sign
 The DNR form should be printed and signed by both the doctor and patient in the presence of two witnesses. These witnesses serve to validate the signatures of the doctor and patient but also to verify that the patient was of sound mind and acting voluntarily when the document was signed (View State Signing Requirements).
The DNR form should be printed and signed by both the doctor and patient in the presence of two witnesses. These witnesses serve to validate the signatures of the doctor and patient but also to verify that the patient was of sound mind and acting voluntarily when the document was signed (View State Signing Requirements).
Both patient and doctor should retain copies of the DNR.
4. Store the Form in a Safe Place
 While a DNR should ensure that a patient is not given CPR in a hospital setting, it may not alter the course of treatment at home. To help ensure that the Do-Not-Resuscitate intention is conveyed, patients are often given a bracelet or other identifying article that would be visible to first responders and others in an emergency non-hospital setting.
While a DNR should ensure that a patient is not given CPR in a hospital setting, it may not alter the course of treatment at home. To help ensure that the Do-Not-Resuscitate intention is conveyed, patients are often given a bracelet or other identifying article that would be visible to first responders and others in an emergency non-hospital setting.
Reasons to Have a Do-Not-Resuscitate Order
While modern medicine continues to advance, patients still find themselves in difficult, even terminal situations. Those who opt for DNRs are often affected by at least one of the following conditions:
- Long-term illness
- Prolonged pain
- Elderly
- Terminally ill
- Dementia
- Alzheimer’s disease
Living Will vs. Do-Not-Resuscitate Order
A living will restricts a patient’s right to food, water, and assisted breathing in a terminally ill state, while a do-not-resuscitate order restricts a patient’s right to immediate life-saving methods such as CPR.
How to Revoke a Do-Not-Resuscitate Order
To revoke a DNR, speak with your doctor. In addition, you should destroy any documentation that asserts the DNR, including bracelets, wallet cards, or other indicators that might be found by emergency personnel.
State Laws & Signing Requirements
A DNR order is required to be authorized in accordance with state law.
| State | Signing Requirements | Laws |
| Alabama | Patient and Physician | § 420-5-19-.02 |
| Alaska | Patient and Physician | AS 13.52.150 |
| Arizona | Patient, Physician, and a Witness | § 36-3251 |
| Arkansas | Patient and Physician | § 20-13 |
| California | Patient and Physician | PROB § 4780 |
| Colorado | Patient and Physician | § 15-18.6-102 |
| Connecticut | Patient and Physician | § 19a-580d |
| Delaware | Patient and Physician | § 2509A |
| Florida | Patient and Physician | FAC 64J-2.018 |
| Georgia | Physician | § 31-39-(2-9) |
| Hawaii | Patient and Physician | § 327K-2 |
| Idaho | Patient and Physician | § 39-4514 |
| Illinois | Patient, Physician, and a Witness | 755 ILCS 40/65 |
| Indiana | Patient, Physician, and 2 Witnesses | § 16-36-5 |
| Iowa | Physician | § 144A.7A |
| Kansas | Patient, Physician, and a Witness | § 65-4943 |
| Kentucky | Patient and Either Two Witnesses or a Notary Public | § 311.623 |
| Louisiana | Patient and Physician | § 40:1155.3 |
| Maine | Patient and Physician | § 93-A.1(b) |
| Maryland | Physician | § 5-608.1 |
| Massachusetts | Patient and Physician | None |
| Michigan | Patient, Physician, and Two Witnesses | § 333.1053 |
| Minnesota | Patient and Physician | Chapter 145C |
| Mississippi | Patient and Physician | § 41-41-302 |
| Missouri | Patient and Physician | § 190.603 |
| Montana | Patient and Physician | § 37:10 |
| Nebraska | Patient, Physician, and a Witness for DNR; Patient and Either Two Witnesses or a Notary Public for Declaration | § 20-404 |
| Nevada | Patient and Physician | § 450B.520 |
| New Hampshire | Patient and Physician | § 137-J:26 |
| New Jersey | Patient and Physician | N.J.A.C. 10:48B |
| New Mexico | Patient and Physician | § 7.27.6.8 |
| New York | Patient and Physician | Senate Bill S7883 |
| North Carolina | Patient and Physician for MOST; Patient, Two Witnesses, and Notary Public for Declaration | § 90-321 & § 90-322 |
| North Dakota | Patient and Physician for POLST | § 23-06.5 |
| Ohio | Physician | § 3701-62 |
| Oklahoma | Patient, Physician, and Two Witnesses | § 63-3131.5 |
| Oregon | Physician for POLST | § 847-035-0030(6) & § 847-010-0110 |
| Pennsylvania | Patient and Physician | § 5481 – § 5488 |
| Rhode Island | Patient and Physician | R23-4.11-MOLST |
| South Carolina | Patient and Physician | § 44-78-10 – § 44-78-65 |
| South Dakota | Patient and Physician | ARSD 44:05:06 & SDCL 34-12F |
| Tennessee | Patient and Physician for POST | § 68-11-224 |
| Texas | Patient, Physician, and Either Two Witnesses or 2nd Physician | § 157.25 & Chapter 166 |
| Utah | Patient and Physician (2nd Physician Required for Minors) | R432-31 |
| Vermont | Patient (if able to sign) and Physician | § 9708 & § 9709 |
| Virginia | Patient and Physician | § 54.1-2987.1 |
| Washington | Patient and Physician for POLST | § 43.70.480 & § 70.245 |
| West Virginia | Patient and Physician for POST | § 16-30C |
| Wisconsin | Patient and Physician | § 154.17 – § 154.29 |
| Wyoming | Patient and Physician | § 35-22-501 – 35-22-509 |