Updated April 04, 2024
An Oregon do not resuscitate (DNR) order form is used to notify medical staff that a patient does not wish to receive cardiopulmonary resuscitation (CPR) when experiencing a medical emergency in which no pulse or breathing is reported. Without a DNR order in place, health care providers will have the responsibility of performing CPR in an attempt to save the patient’s life. The DNR order can be requested from the patient’s doctor or from another authorized individual. The order shall be signed by the patient and the authorized medical professional.
Laws – § 847-035-0030(6) and § 847-010-0110
Required to Sign (POLST) – MD/DO/PA/NP (signature of the patient is recommended).
The State provides no official DNR order form. However, Oregon has a Physician Orders for Life-Sustaining Treatment (POLST) program which permits patients to use a similar form to specify the treatments they desire during medical emergencies. The document used for this purpose, the “POLST” form, must be requested from the patient’s doctor or directly from the Oregon POLST program.
Note: The instructions provided below are directed towards the completion of an Oregon POLST form. The downloadable document is a sample only. A newer version of the form may be available. Ensure that you obtain the latest version from your doctor or from the Oregon POLST program.
How to Write
Step 1 – Download the sample Oregon POLST form in PDF.
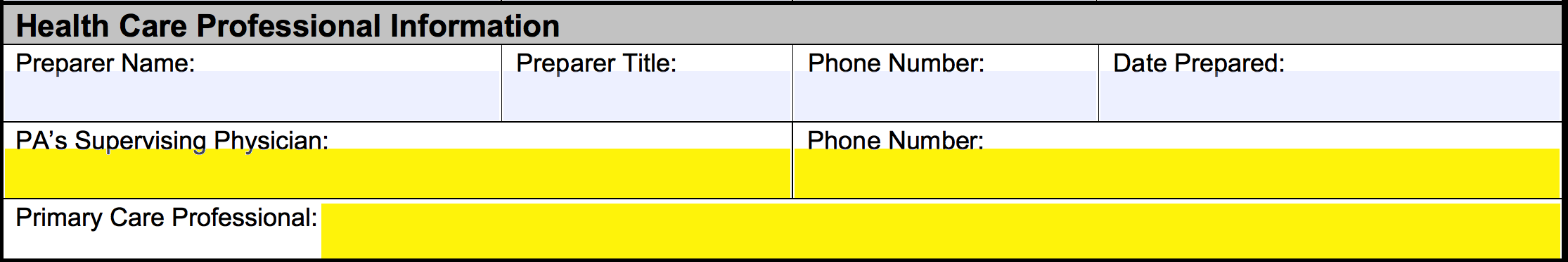
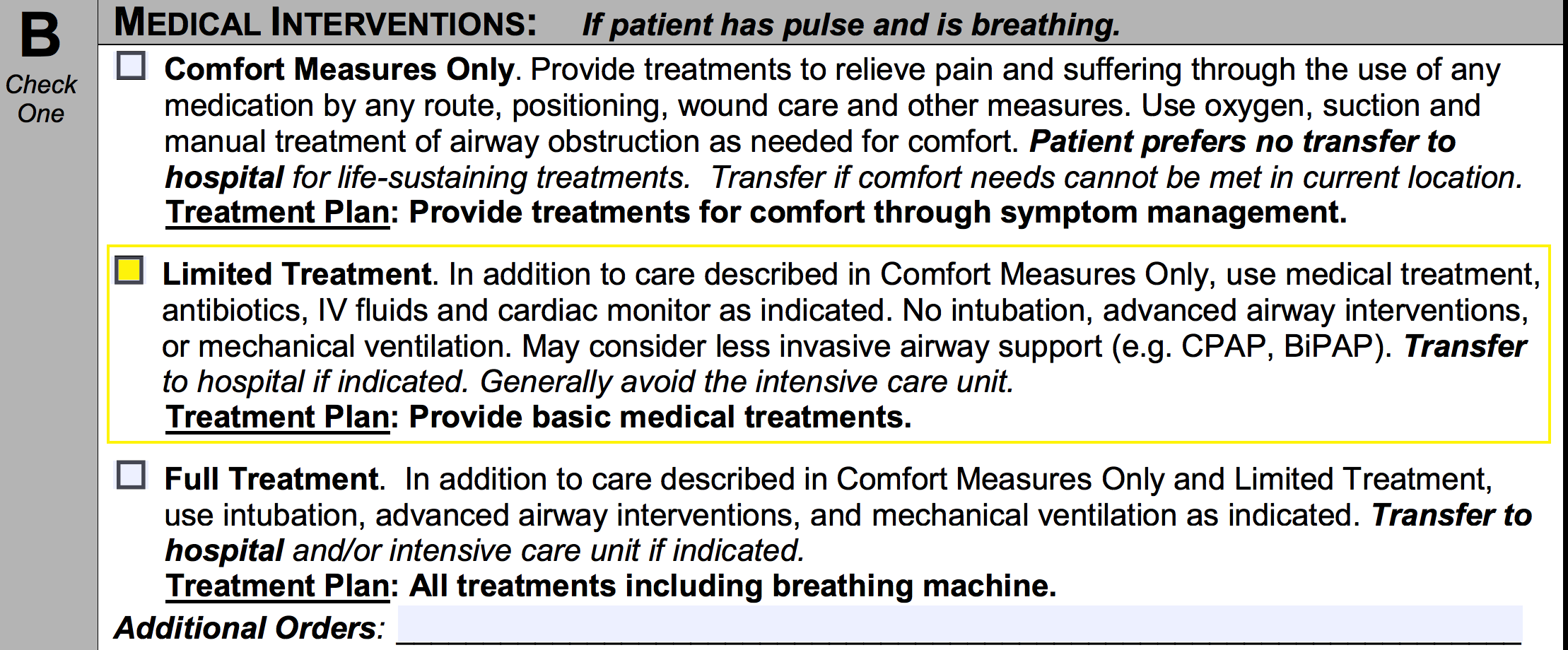
Step 2 – In the first set of empty spaces, enter the patient’s last name, first name, last (4) digits of SSN, address, date of birth (mm/dd/yyyy), and gender.
Step 2 – Continue to section A and select one (1) of the two (2) available boxes to indicate whether or not the patient wishes to be resuscitated in the event that they are unresponsive, pulseless, and not breathing. If the patient would like to be resuscitated, select the first checkbox. If the patient does not wish to be resuscitated, the second box should be selected.
![]()
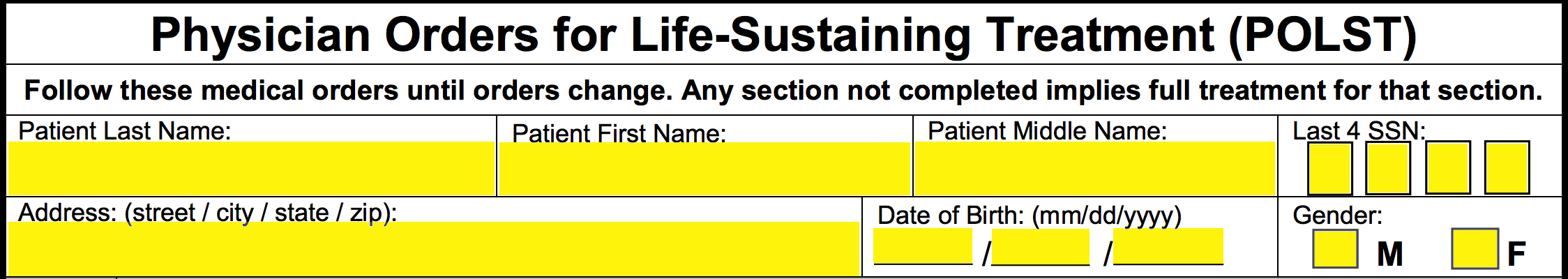
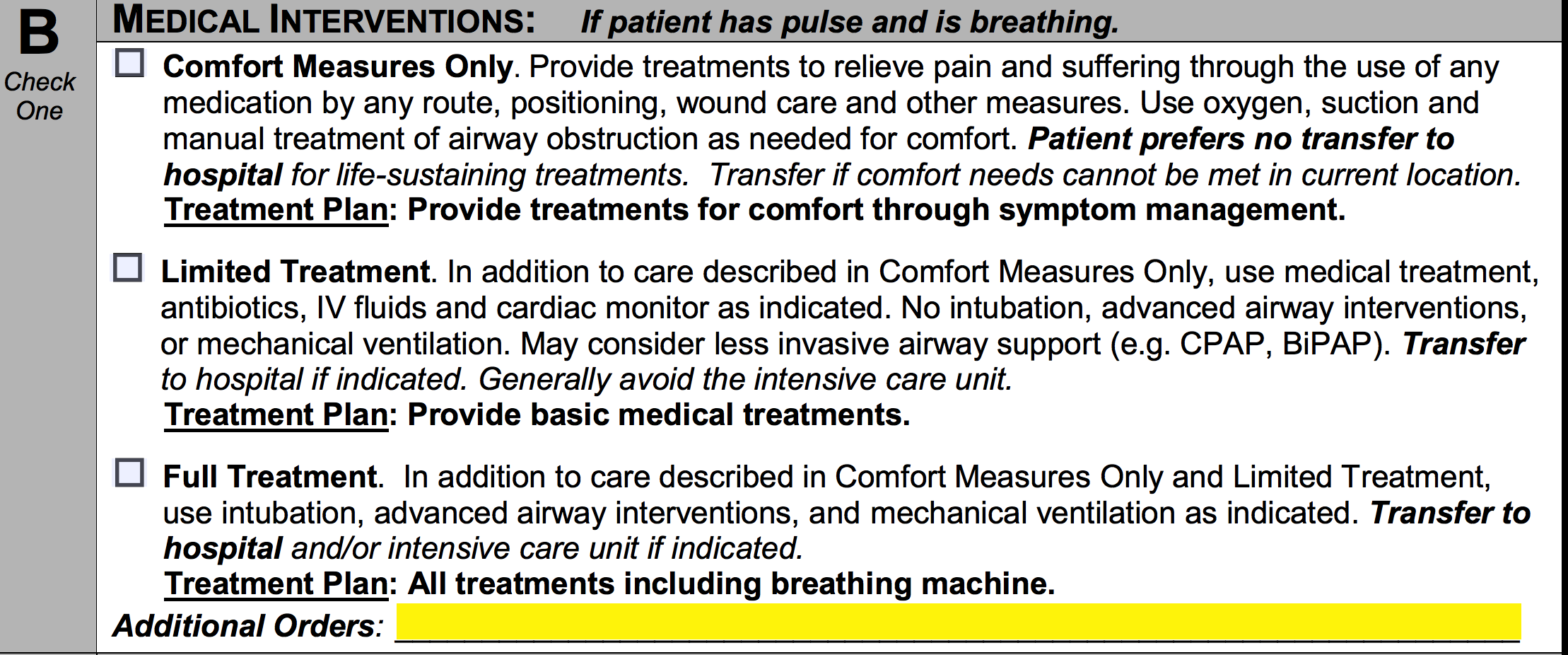
Step 3 – Section B allows the patient to further define the treatments which are to be administered in the event that they are ill but continue to breathe and maintain a pulse. Only one (1) of the options may be selected.
The first option, “Comfort Measures Only,” should be selected if the patient wishes to receive treatments to relieve pain through the application of medication by any route, positioning, wound care or other means. This includes the use of oxygen, suction, and manual clearing of the airway. Furthermore, this option indicates the patient’s desire to not be transferred to a hospital for life-sustaining treatments unless their comfort is in jeopardy at their current location.
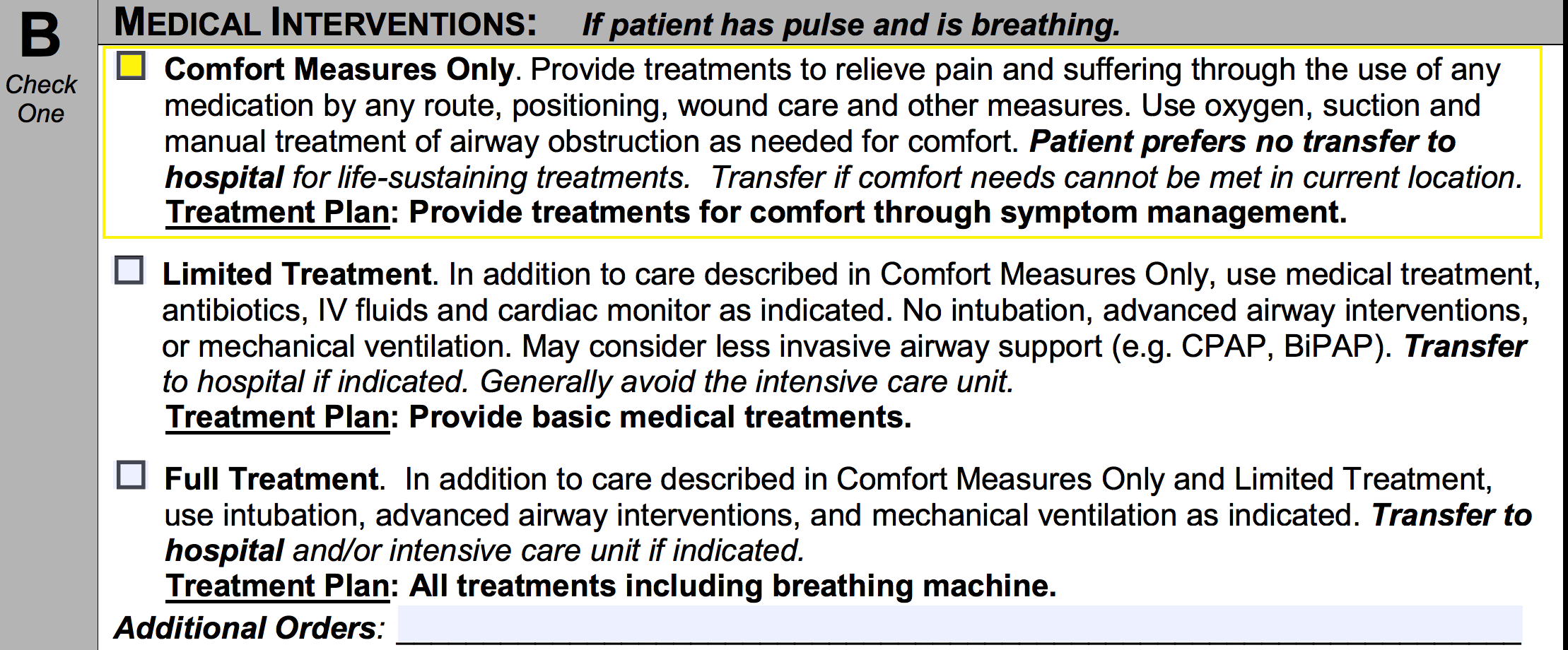
The second option, “Limited Treatment,” should be selected if the patient would like to receive, in addition to the treatments of “Comfort Measures Only,” medical treatments, IV fluids, antibiotics, and cardiac monitoring. This option specifies the patient’s desire to receive no mechanical ventilation, intubation, or advanced airway interventions. Transfer to a hospital (preferably without intensive care) is accepted through this option.
The final option, “Full Treatment,” should be selected if the patient wishes to receive the treatments defined in both “Comfort Measures Only” and “Limited Treatment.” This option also specifies the patient’s desire to allow intubation, mechanical ventilation, and advanced airway interventions. Transfer to a hospital and/or the intensive care unit is permitted.
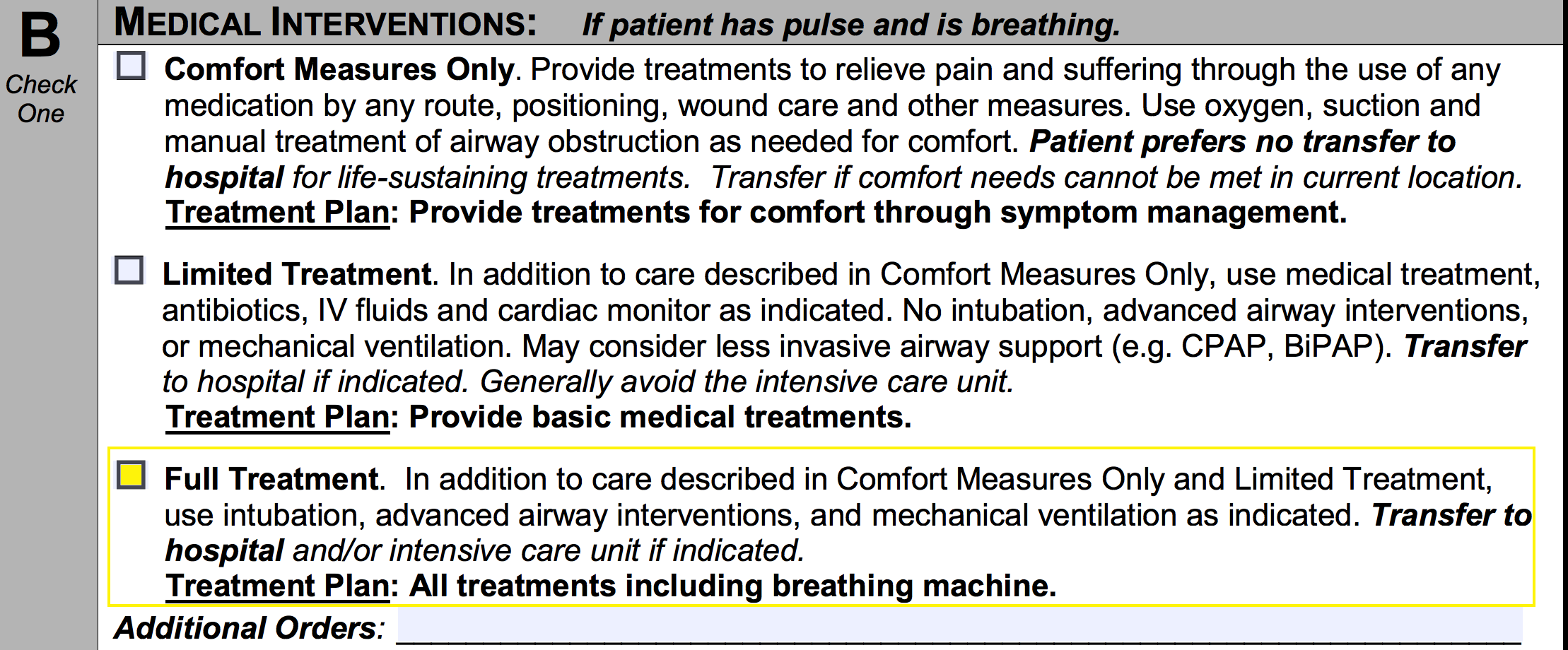
Step 4 – Complete section B by mentioning any additional orders the patient wishes to receive.
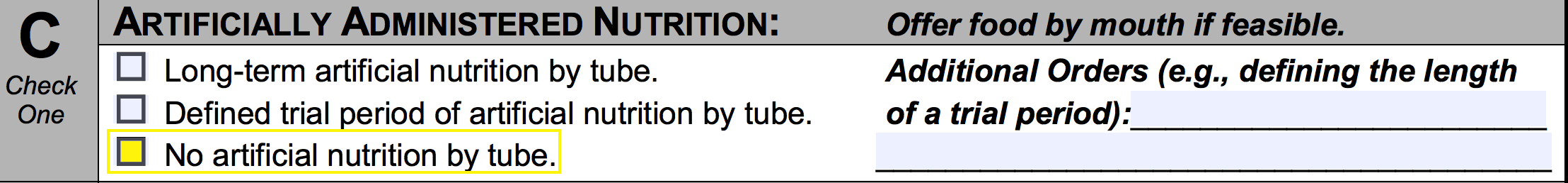
Step 5 – In section C, choose one (1) of the boxes to indicate the patient’s desired method of artificially administered nutrition.
Select the first box if the patient would like to receive long-term artificial nutrition by tube.
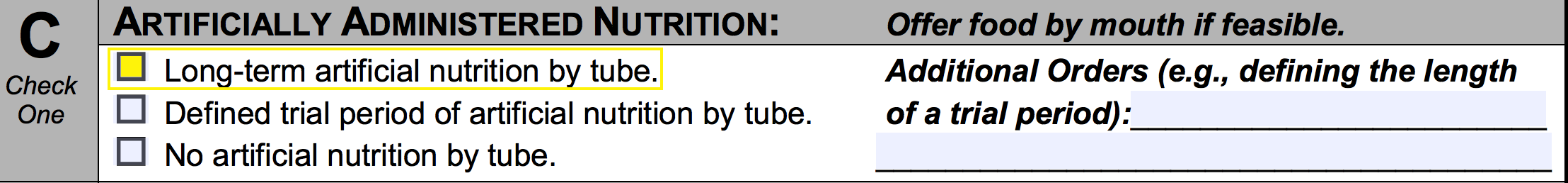
Select the second box if the patient desires to receive artificial nutrition by tube for a defined length of time. Specify the amount of time in the empty spaces on the right.
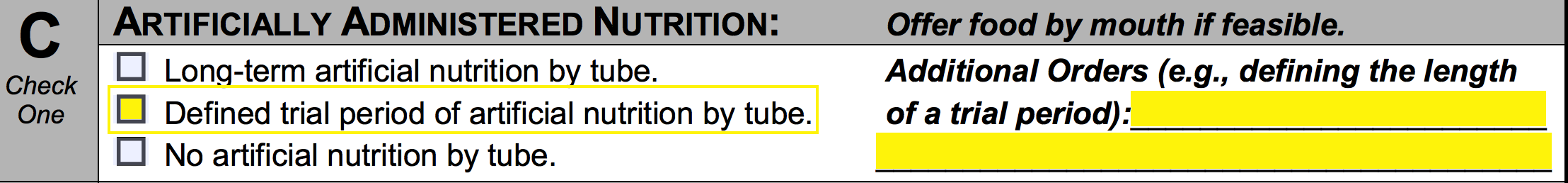
If the patient does not want to receive artificial nutrition by tube, the final checkbox should be selected.
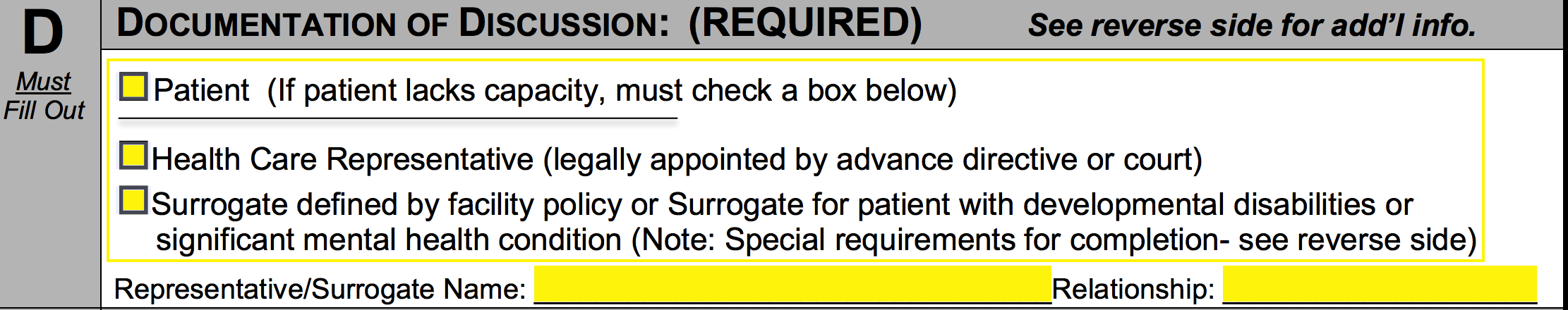
Step 6 – In section D, you’ll need to indicate the circumstance under which this document is being executed. Select the first box if the POLST was requested by the patient. Select the second box if the POLST was requested by a health care representative who is legally appointed to act on the patient’s behalf. If a surrogate has been chosen for the patient, select the final box and enter the individual’s name and their relationship to the patient.
Step 7 – The patient should provide their signature in section E (not required). If the patient does not wish to have this form sent to the POLST registry, select the box on the right.
![]()
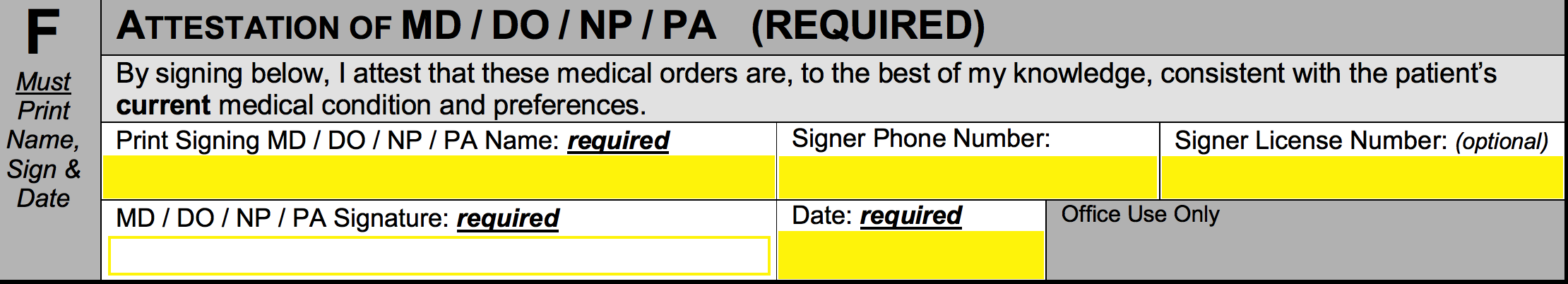
Step 8 – In section F, the individual authorized to execute this document must print their name, enter their phone number, and give their license number (optional). They must then supply the signature and specify the date of signing.
Step 9 – Proceed to the second page and enter the patient’s name in the first available space.
![]()
Step 10 – The contact information of the health care representative or surrogate may be entered below the “Contact Information (Optional)” heading. In the empty spaces, enter the individual’s name, relationship to the patient, phone number, and address.
![]()
Step 11 – Below the “Health Care Professional Information” heading, you may optionally enter the name, title, and phone number of the person who prepared this form, followed by the date the form was executed.
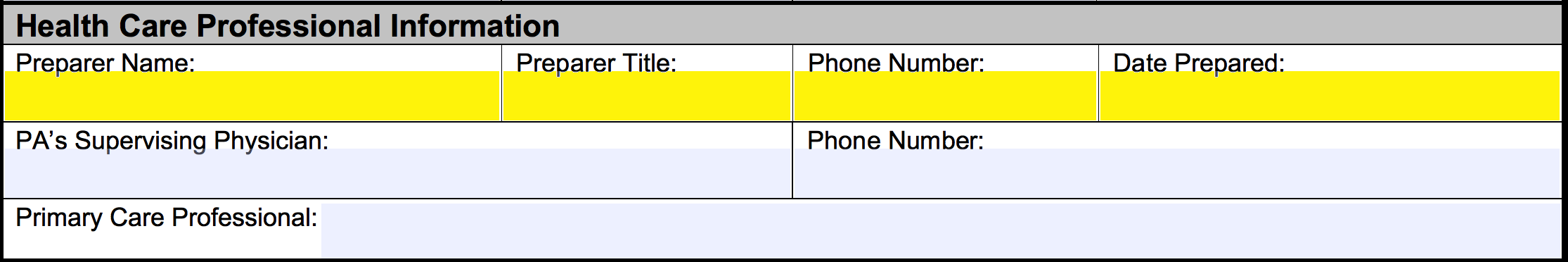
Step 12 – Lastly, below the “Health Care Professional Information” heading, you can provide the name and phone number of the PA’s supervising physician. The final space can be filled in with the name of the primary care professional.