Updated July 19, 2023
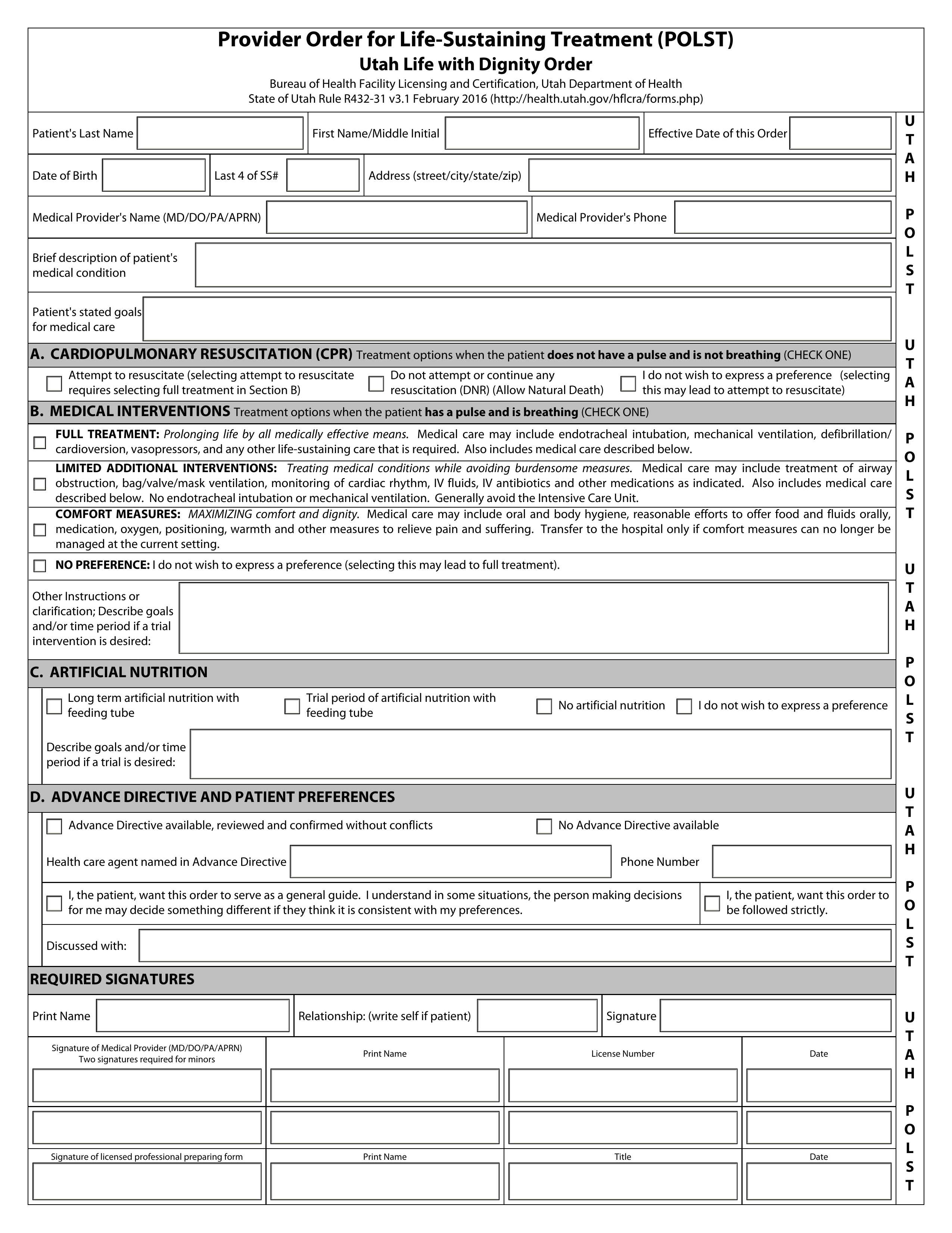
A Utah do not resuscitate (DNR) order form tells emergency medical personnel not to attempt cardiopulmonary resuscitation (CPR) on a patient who is experiencing cardiac or respiratory failure. This type of order is critical in avoiding invasive and unwanted treatments which would typically be applied during a medical emergency. The patient can verbally request a DNR order from their physician, or they can make a written request in their advance directive or living will.
A more comprehensive version of a DNR form has recently been implemented in Utah. This document, known as the “POLST” form (Provider Order for Life-Sustaining Treatment), informs emergency medical service providers of the patient’s desired resuscitative treatments, as well as medical interventions to be applied when the patient maintains a pulse and/or can still breathe. Follow the instructions below to complete a Utah POLST form.
Laws – R432-31
Required to Sign (POLST) – MD/DO/PA/APRN, and patient (or representative).
How to Write
Step 1 – Download the Utah POLST form in PDF.
Step 2 – The first set of fields must be filled in with some general information relating to the patient and the effective date of the POLST order. In the blank spaces, enter the patient’s last name, first name/middle initial, date of birth, last four (4) digits of SSN, and address. The effective date of the order must be entered in the remaining space.
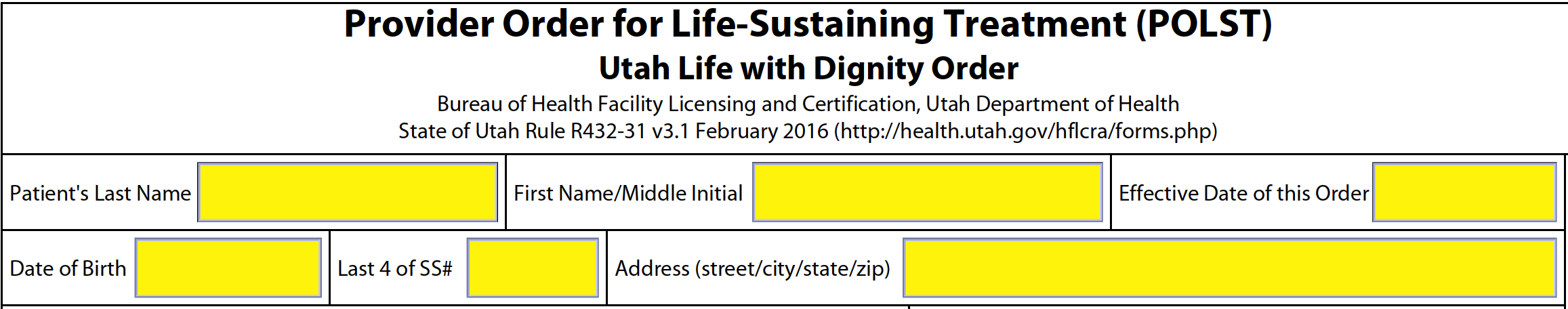
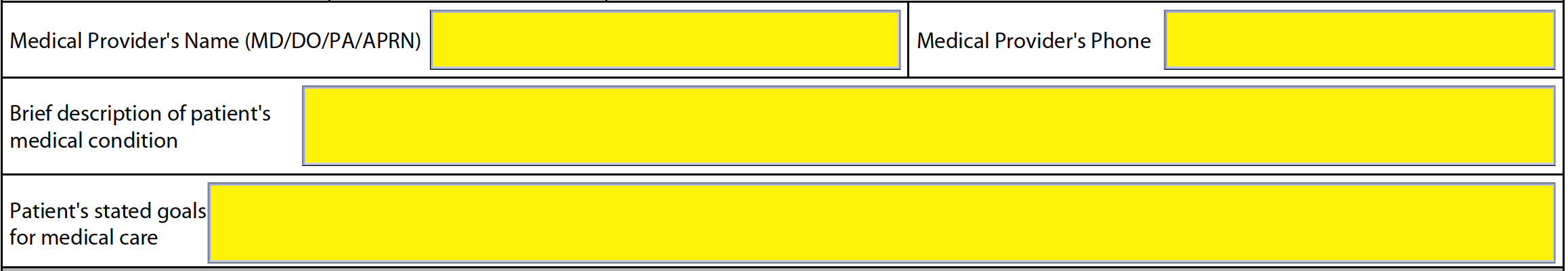
Step 3 – Next, the health care provider must supply the following information:
- Full name
- Phone number
- Brief description of the patient’s medical condition
- Medical goals stated by the patient
Step 4 – In Section A, you will need to select one (1) of the boxes to indicate the resuscitative treatments which should be applied (if any) when the patient has no pulse and is not breathing. The options are as follows:
- Attempt to resuscitate
- Do not attempt or continue resuscitation
- No preference
![]()
Step 5 – Select one (1) of the boxes in section B to indicate the desired treatment options applied when the patient has a pulse and is breathing.
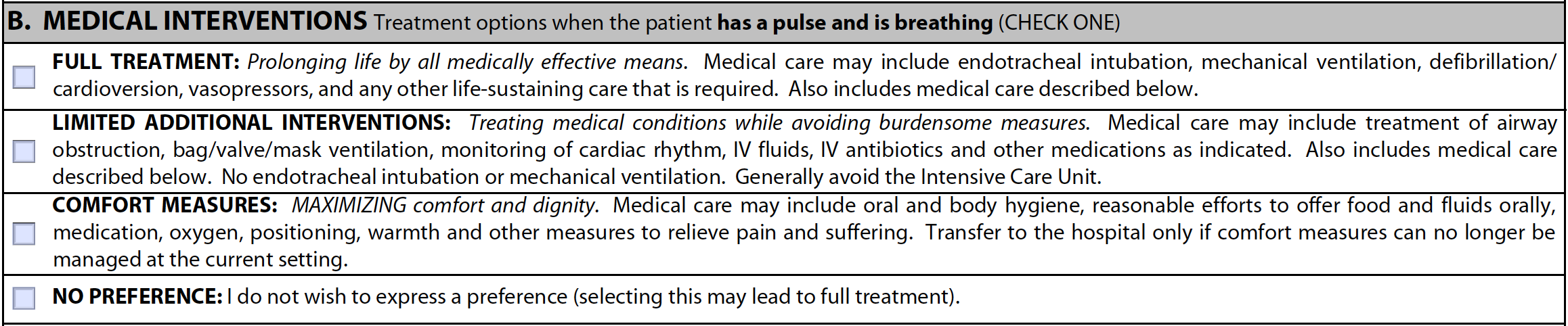
Choose “FULL TREATMENT” if the patient should have their life prolonged by all effective medical means. This option includes the treatments offered in the each of the medical interventions mentioned in section B.
![]()
Choose “LIMITED ADDITIONAL INTERVENTIONS” if the patient should have their medical conditions treated while avoiding care which might be a burden. This option includes the treatments offered in Comfort Measures Only.
![]()
Choose “COMFORT MEASURES ONLY” if the patient should be treated to maximize their dignity and comfort which may include being transferred to the hospital if necessary.
![]()
Select “NO PREFERENCE” if the patient or their representative does not wish to specify any treatments (this may result in full treatment of the patient).
![]()
Finally, enter any additional instructions that the patient may require (e.g., trial intervention period, treatment goals, etc.).
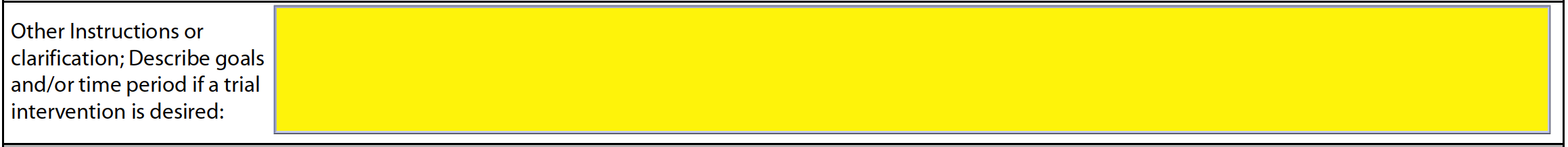
Step 6 – Select one (1) of the boxes in section C to specify the type of artificial nutrition the patient should receive (if any). The following options are available:
- Long-term artificial nutrition with feeding tube
- Trial period of artificial nutrition with feeding tube
- No artificial nutrition
- No preference
If a trial period of artificial nutrition is required, specify the goals of the treatment as well as the time period.
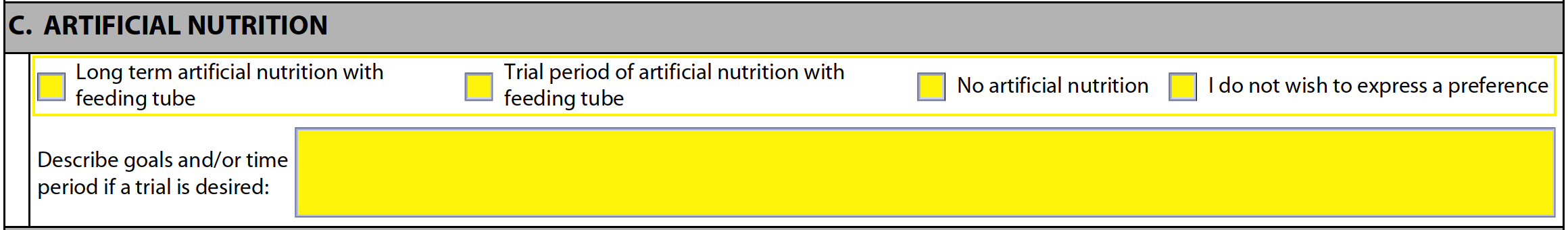
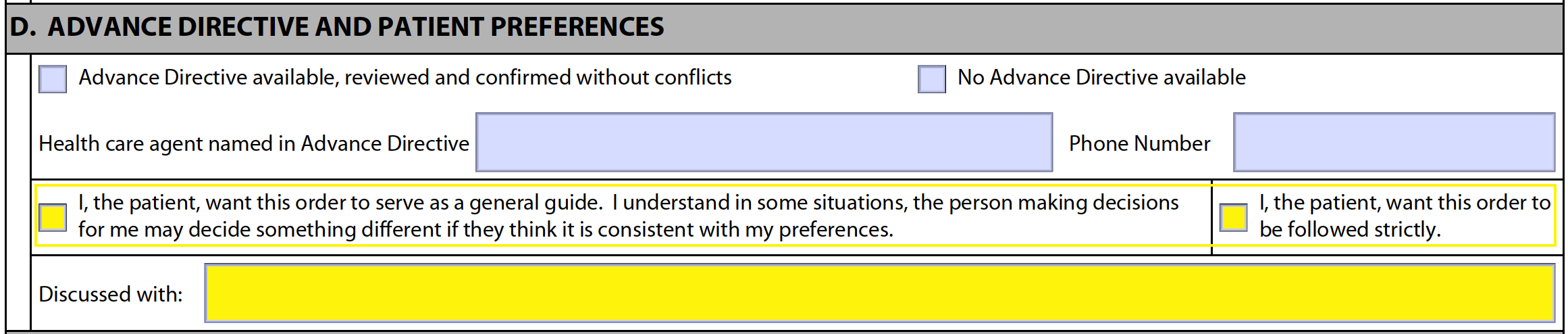
Step 7 – Begin filling in section D by specifying whether or not an advance directive is available (choose one (1) of the boxes). Below that, enter the name of the health care agent named in the advance directive along with their phone number (if applicable).
Step 8 – Also in section D, select one (1) of the boxes to indicate whether the patient would like the instructions of their POLST followed as a general guide, or if it should be followed strictly. Below that, specify who had discussed the POLST order with the attending physician.
Step 9 – Below “REQUIRED SIGNATURES,” the patient or authorized representative must print their name, specify their relationship to the patient (if the patient is signing, write “self”), and provide their signature.
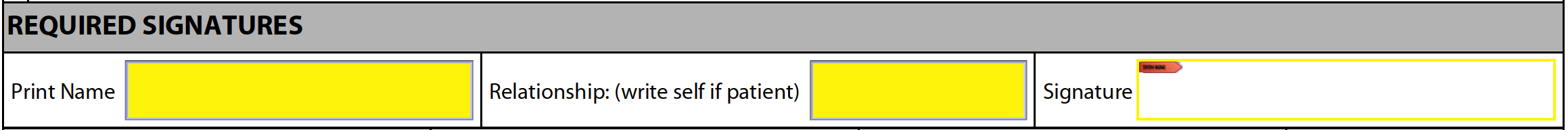
Step 10 – Next, the attending health care professional must supply their signature, printed name, license number, and the date. If the patient is a minor, a second health care professional must provide the same information.
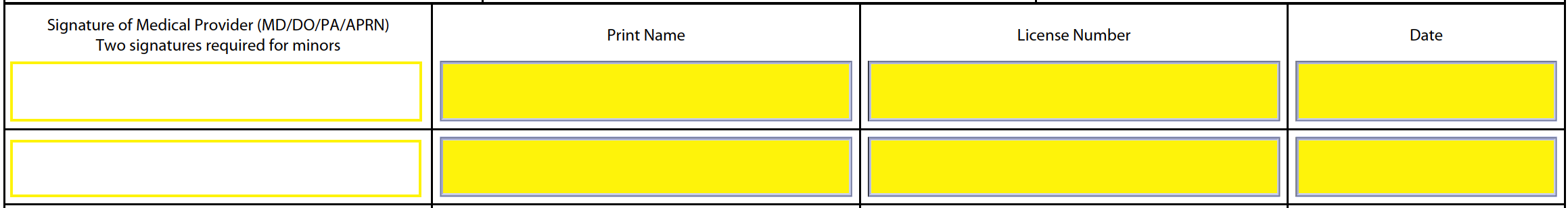
Step 11 – Finally, the name of the licensed health care professional who prepared this form must sign, print their name, enter their title, and record the date.
![]()