Updated July 19, 2023
The Tennessee do not resuscitate (DNR) order form informs emergency medical service providers that no cardiopulmonary resuscitation (CPR) should be initiated on a patient. An applicant for a Tennessee DNR order must be diagnosed with a terminally ill condition in order for the attending physician to execute the form. Once the form is effective, the patient will not be resuscitated in the event of a medical emergency where their breathing or heart ceases to function.
Tennessee has updated their health care regulations regarding end-of-life and emergency resuscitative treatments. They have adopted the Physician Orders for Scope of Treatment (POST) program which, like a DNR order, allows patients to specify whether or not CPR should be administered during medical emergencies. The POST program also enables patients to define the treatments they desire when they can still breathe or while a pulse is maintained.
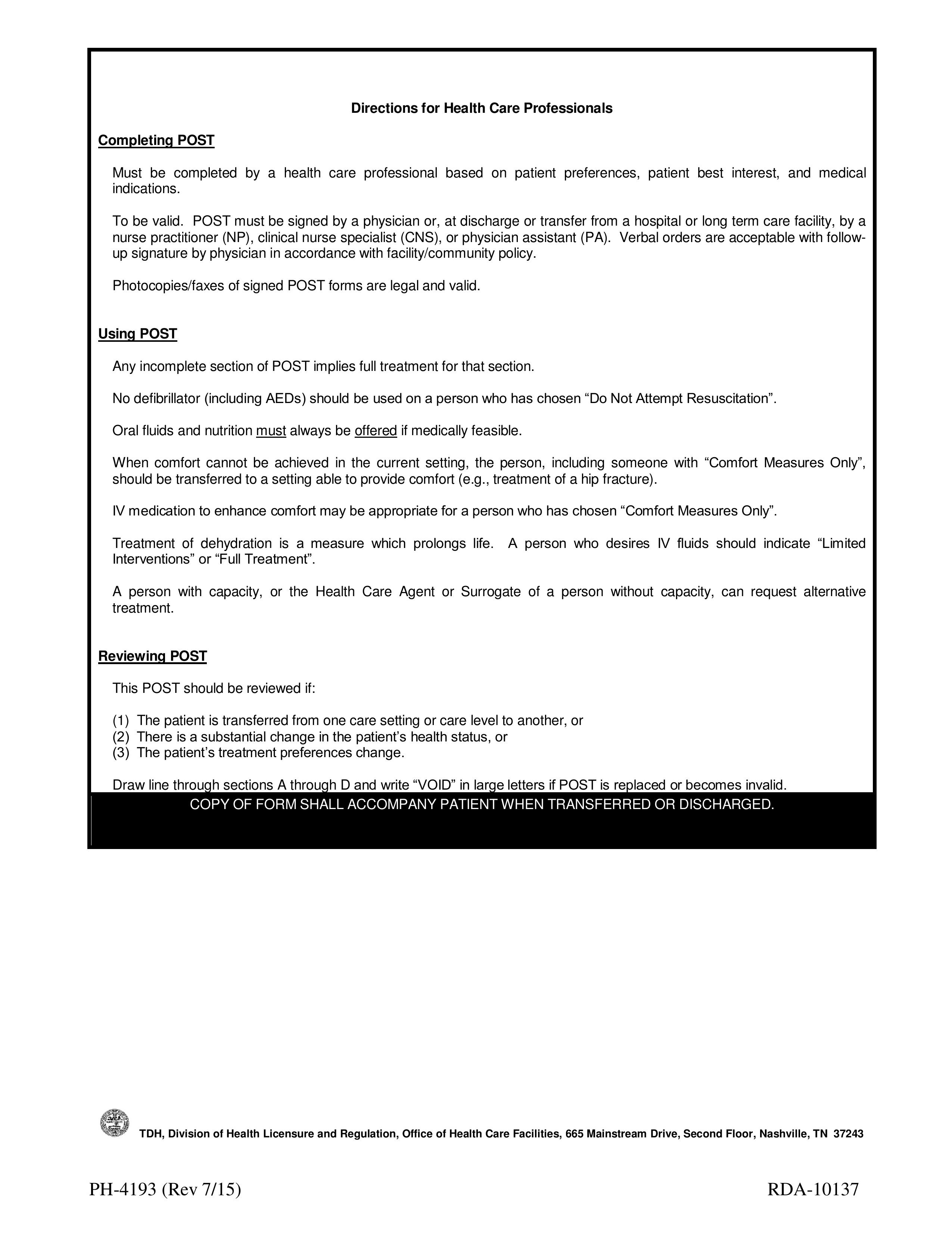
Contact a medical professional for information on how to properly execute a Tennesee Do Not Resuscitate (DNR) Order Form. Alternatively, you can follow the instructions below to complete the POST application.
Laws – § 68-11-224
Required to Sign (POST) – MD/NP/CNS/PA, and patient (or representative).
How to Write
Step 1 – Download the Tennessee POST form in PDF.
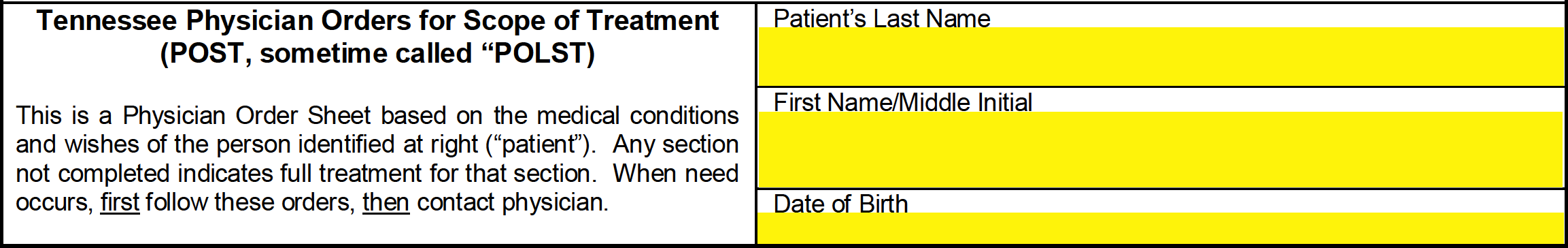
Step 2 – Proceed to the second page of the POST form. In the spaces at the top of the page, enter the patient’s last name, first/middle name, and date of birth.
Step 3 – The two (2) checkboxes in section A are used to indicate whether or not the patient wishes to be resuscitated when they have no pulse or are not breathing. Only one (1) of the boxes must be selected.
Choose “Resuscitate (CPR)” if the patient should be resuscitated.
![]()
Choose “Do Not Attempt Resuscitation (DNR / no CPR) (Allow Natural Death)” if the patient should not be resuscitated.
![]()
Step 4 – Section B is used to specify the treatments applied when the patient has a pulse or is breathing. Only one (1) of the three (3) options may be selected.
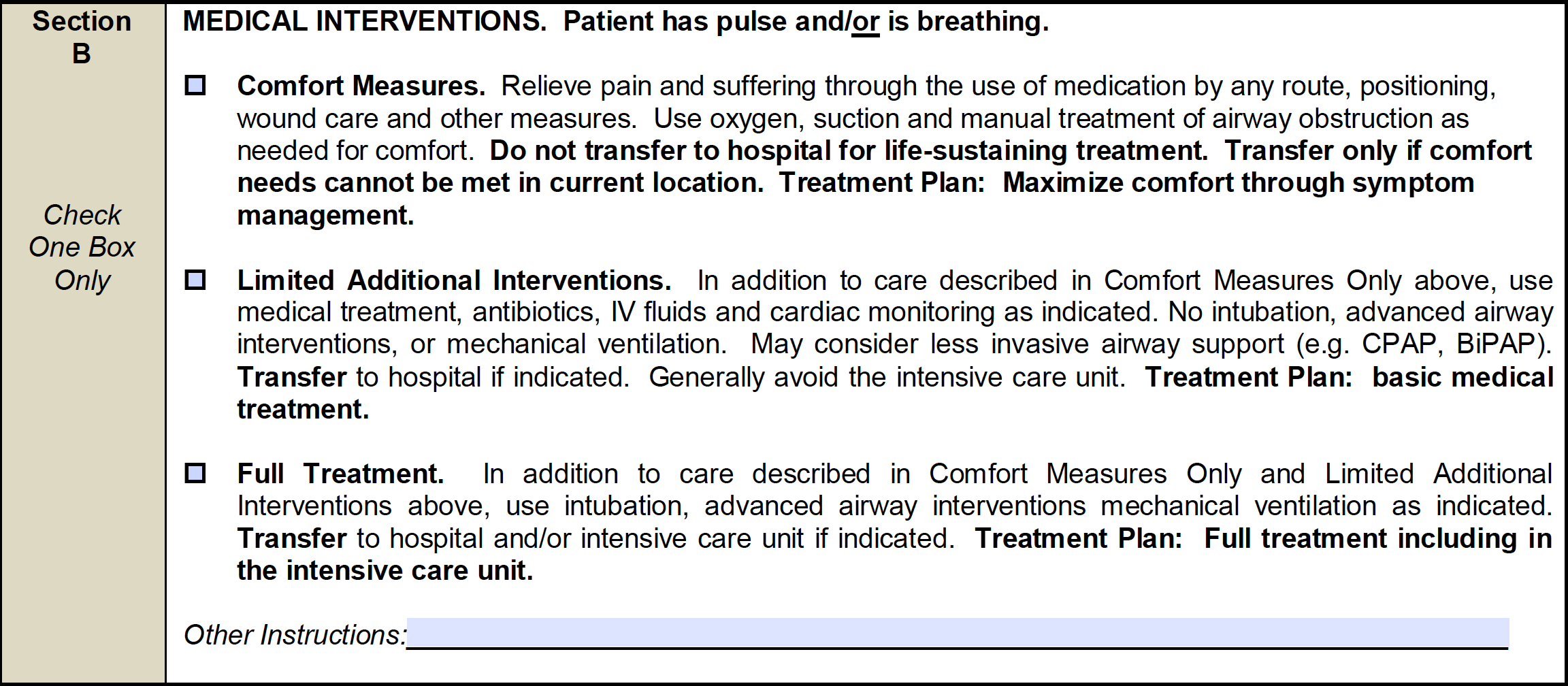
Select “Comfort Measures” if the patient should receive basic treatment to relieve pain and suffering.
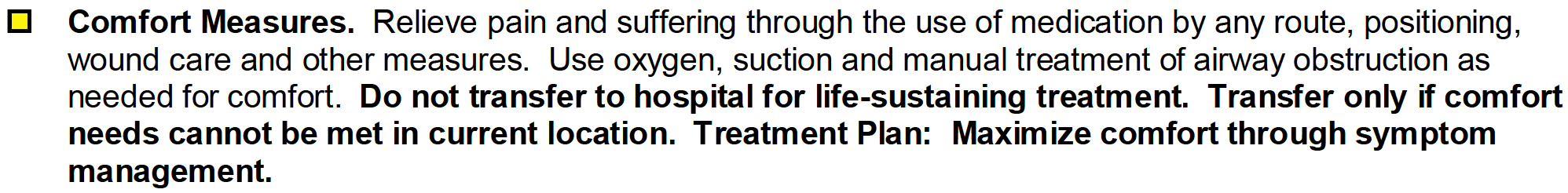
Select “Limited Additional Interventions” if the patient should be given medical treatment in addition to the treatments provided in Comfort Measures Only.
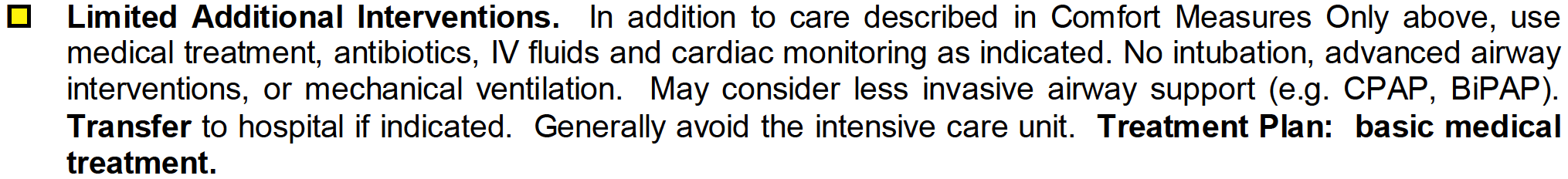
Choose “Full Treatment” if the patient should receive the care provided in both Comfort Measures Only and Limited Additional Interventions. This option includes intubation, mechanical ventilation, and transfer to the hospital and/or intensive care if required.
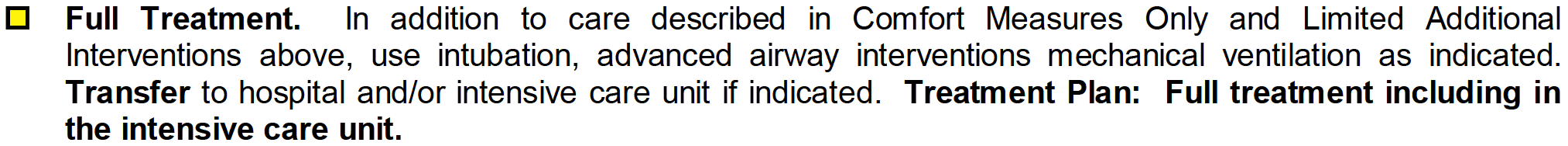
Any additional provisions may be entered in the space next to “Other Instructions.”
![]()
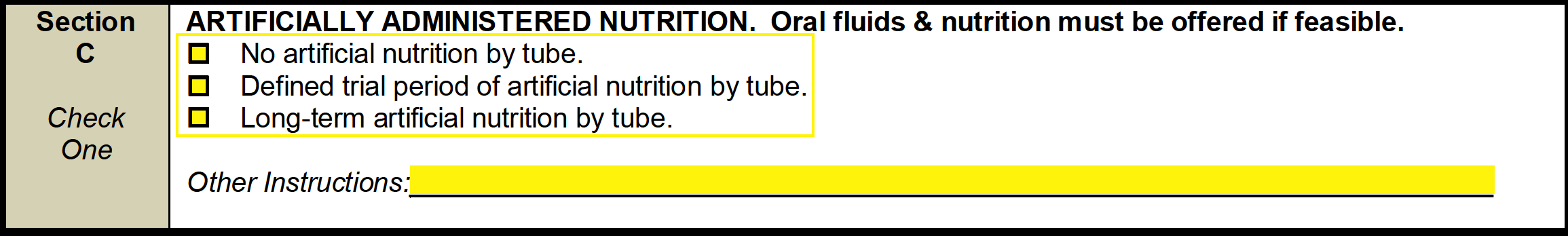
Step 5 – Select one (1) of the three (3) available boxes in section C to specify the requested method of artificially administered nutrition (if any). The choices are as follows:
- No artificial nutrition by tube
- Defined trail period of artificial nutrition by tube
- Long-term artificial nutrition by tube
Use the remaining space to enter any additional instructions.
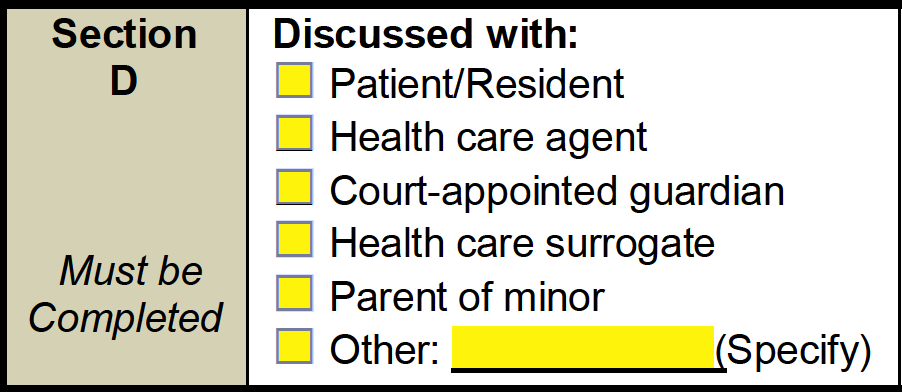
Step 6 – In section D, select one (1) of the following options to specify who requested the POST form:
- Patient/Resident
- Health care agent
- Court-appointed guardian
- Health care surrogate
- Parent of minor
- Other (specify)
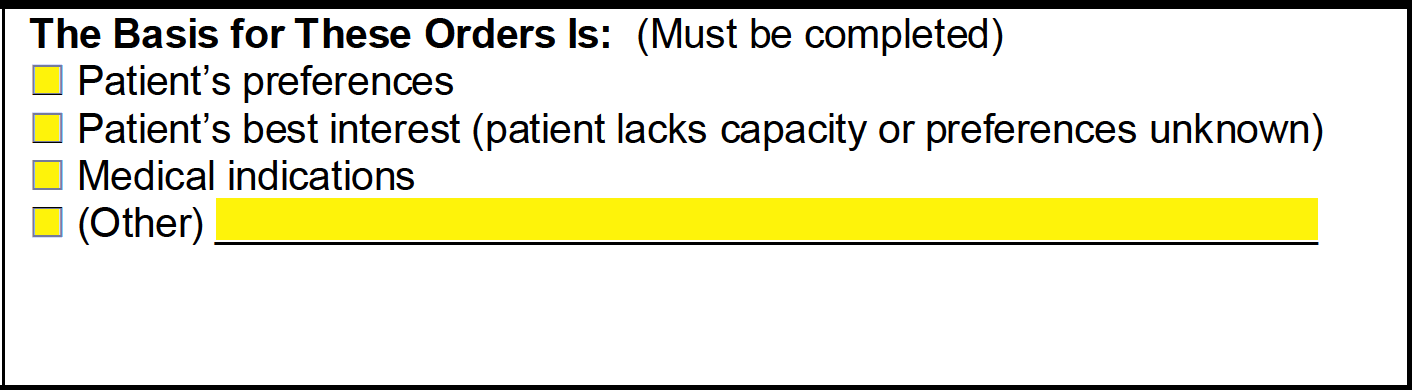
Step 7 – In the right portion of section D, indicate the reason for the POST form by selecting one (1) of the following options:
- Patient’s preferences
- Patient’s best interest
- Medical indication
- Other (specify)
Step 8 – In the spaces below section D, the health care provider must print their name and provide their signature. The individual must then enter the date the form was executed along with their phone number.
Note: The “Signature at Discharge” field should only be signed by a health care provider when the patient is discharged or transferred from a hospital.
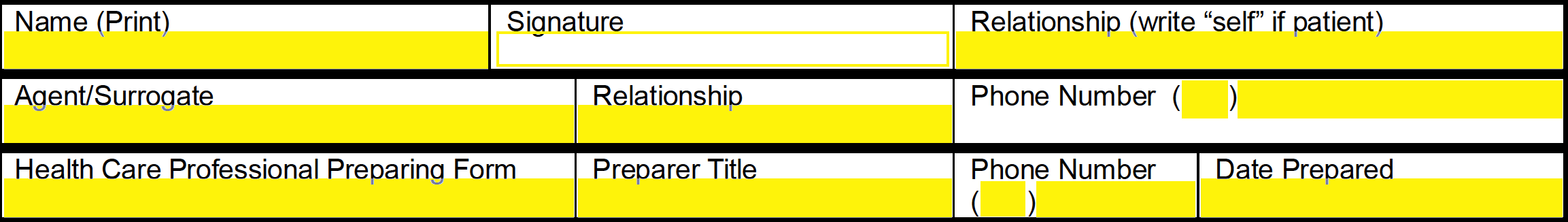
![]()
Step 9 – The remaining spaces will be used to input the patient/authorized representative’s information. The individual must enter their name, signature, and their relationship to the patient (if the patient is signing, write “self”). If there is a surrogate/agent, specify their name, relationship to the patient, and their phone number. Lastly, enter the name of the health care professional who prepared the form, their professional title, phone number, and the date the form was prepared.