Updated July 19, 2023
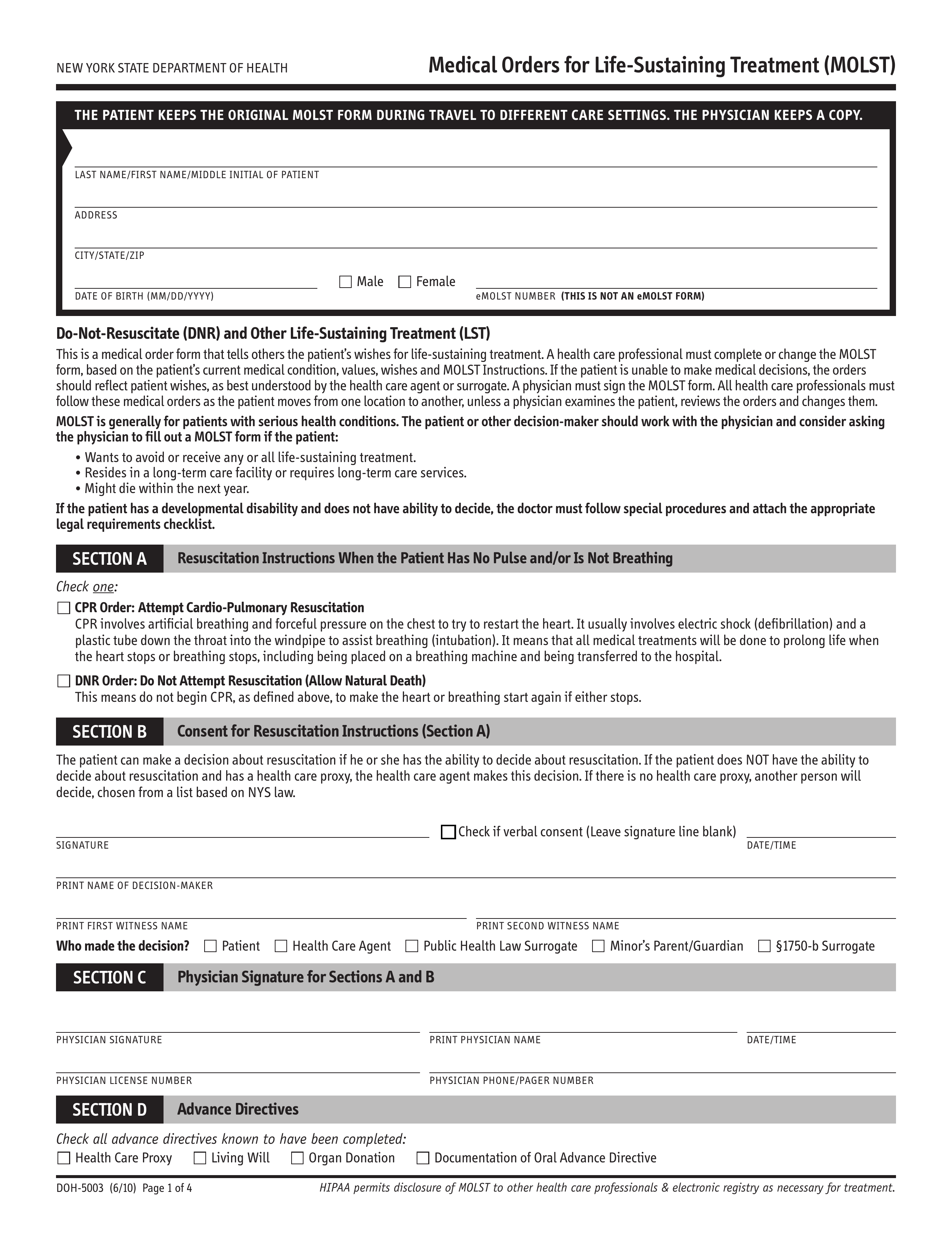
The New York Medical Orders for Life Sustaining Treatment (MOLST) helps to specify a patient’s wishes regarding life-sustaining treatments and is often used by those who are in the critical stages of an illness or old age. If a MOLST is indicated in the patient’s medical record, they will not be given cardiopulmonary resuscitation (CPR) in the event of a cardiac/respiratory arrest. This form details multiple aspects of end-of-life care and is recognized by all healthcare professionals in the State. Physicians may also fill out the electronic version of the form by using the eMOLST web service.
Laws – Senate Bill S7883
Required to Sign – Both the patient (or their representative) and the attending physician must sign. Also requires the printed names of two (2) witnesses.
Spanish (Español) Version – PDF
How to Write
Step 1 – Download in PDF.
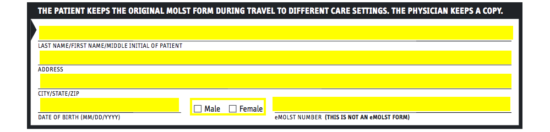
Step 2 – There are four (4) pages of the MOLST form. Enter the full name, address, date, gender, and eMOLST number (if applicable) of the patient at the top of the first page.
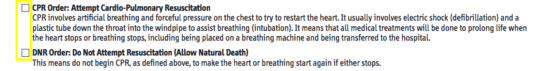
Step 3 – At this juncture, you will indicate whether a CPR Order or a DNR Order is issued in this document by checking the appropriate box.
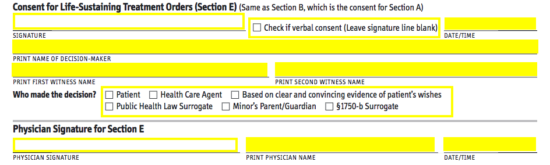
Step 4 – Supply the patient’s signature or check the box indicating that they gave their verbal consent. Next to that, enter the date and time of issuance. Below that, provide the names of the decision maker and the two (2) required witnesses. Next, check the appropriate box to indicate who made the decision to authorize this form (patient, health care agent, surrogate, or parent/guardian).
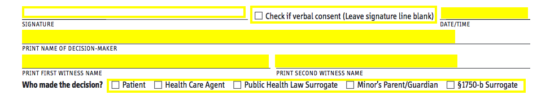
Step 5 – In Section C, the physician must provide their signature, name, license number, and phone/pager number, along with the date and time.
Step 6 – Under “Advanced Directives,” indicate what types of advance directives the patient is known to have filed.
![]()
Step 7 – At the top of the second page, enter the full name of the patient and their date of birth.

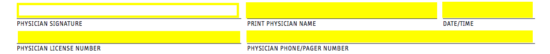
Step 8 – Next, you will need to select the appropriate checkboxes to indicate the following:
- What forms of treatment will be permitted
- If the patient should be intubated (connected to a breathing machine); if so, indicate the duration
- If the patient should be transferred/sent to a hospital or not
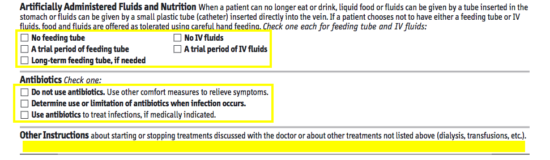
Step 9 – Indicate whether or not the patient should be administered fluids and nutrition by feeding a tube and/or IV fluids, or if only a trial period is permitted. Below that, select one option for how antibiotics may be administered and write any further instructions beneath “Other Instructions.”
Step 10 – In Section E, the patient or authorized representative will need to provide their signature (or you will need to tick the box indicating that their verbal consent was given). You will also need to provide the date of signing, the printed name of the “decision maker,” along with the printed names of the two (2) witnesses. Next, indicate who the “decision maker” is and supply the attending physician’s signature and name, along with the date.
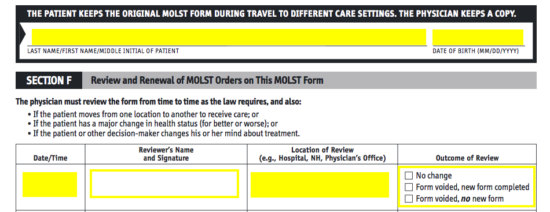
Step 11 – At the top of the third and fourth pages, the name and date of the patient must be entered. These pages are to be kept and filled-in each time the MOLST form is reviewed. Everytime that the patient is moved to a new facility, has a major change in health, or if they change their mind about treatment, the MOST form will be reviewed for its necessity and alignment with the patient’s wishes or condition. The reviewer will need to supply the date and time, their signature, the facility/location, and the outcome of the review.