Updated July 19, 2023
The North Carolina do not resuscitate (DNR or DNAR) order form serves residents who wish to order medical personnel not to administer CPR on them if they have a cardiac or respiratory arrest. In accordance with the Right to Die a Natural Death Act (Article 23), a declaration to disallow the use of CPR or other life-prolonging measures can be made by anyone who suffers from an irreversible condition, or who becomes permanently unconscious or suffers from a substantial loss of cognitive ability. This type of declaration, or advanced directive, must be signed in the presence of two (2) witnesses and notarized.
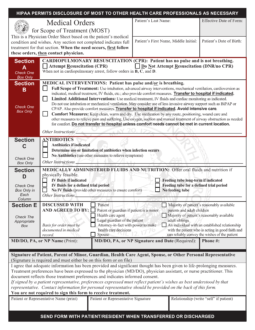
To ensure that a patient’s desires are properly met, a physician can issue a DNR order or a Medical Orders for Scope of Treatment (MOST) form. Once issued, these forms are kept with the patient’s medical record, usually printed on brightly colored paper. The MOST form covers the DNR order in addition to a variety of other end-of-life treatments and informs all medical personnel of how to honor the wishes of the patient. This form does not replace a declaration, rather, it translates the patient’s wishes into a medical order which will stay with the patient in the event that they are transferred from one facility to another. If the patient is incapacitated or otherwise impaired, their authorized medical decision-maker may sign the MOST form on their behalf.
Laws – § 90-321 and § 90-322
Required to Sign – Patient (or a representative) and the attending physician must sign (for a MOST form); patient and two (2) witnesses must sign, with notarization (for a declaration).
Spanish (Español) Version – PDF
How to Write
Step 1 – Download the North Carolina MOST Form.
Step 2 – Enter the last name, first name, and middle initial of the patient, along with the date that the form becomes effective.
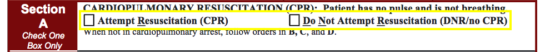
Step 3 – Section A covers the DNR order. Check the appropriate box to indicate whether or not the patient wishes to receive CPR.
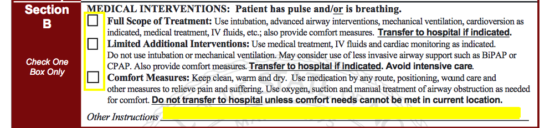
Step 4 – In Section B, select one (1) of the three (3) options for what kind of medical interventions shall be authorized if the patient is breathing and/or has a pulse.
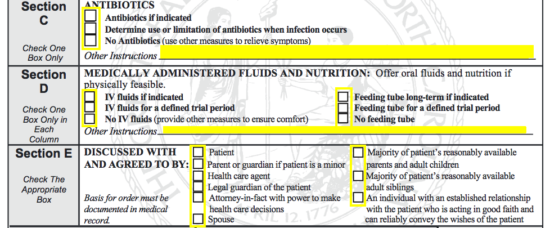
Step 5 – Next, you will need to indicate which kind of antibiotics and medically administered fluids and nutrition will be permitted in treatment, writing any additional instructions in the blank space(s). Below that, check the appropriate box(es) to indicate who the contents of this form have been discussed with.
Step 6 – Provide the name, signature, date, and phone number of the attending physician.
![]()
Step 7 – Enter the name of the patient or their representative and supply their signature. Beside those fields, write the representative’s relationship to the patient (write “self” if it is the patient).
![]()
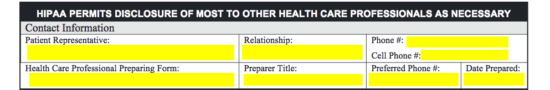
Step 8 – At the top of the second page, you must provide the following contact information:
- Name of patient representative
- Relationship of representative to patient
- Representative’s phone and cell phone numbers
- Name of health care professional preparing form
- Preparer’s title
- Preparer’s telephone number
- Date of the form’s preparation
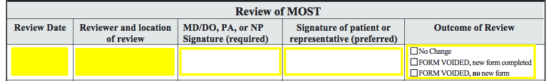
Step 9 – The MOST form will be reviewed periodically and when the patient moves from one facility to another. At each reviewal, the date, reviewer, location, and the signatures of the physician and the patient (or their representative) must be provided. Beneath “Outcome of Review,” it will be indicated whether the form will be voided, replaced, or if there will be no change.