Updated July 19, 2023
A Rhode Island medical orders for life-sustaining treatment (MOLST) alerts health care professionals that a patient does not wish to be brought back to life through the administration of cardiopulmonary resuscitation (CPR). This type of medical order will only be effective during an emergency where the patient’s heart or breathing stops. The attending health care professional must view the MOLST order immediately or resuscitative measures will be performed.
The form available below should be used by a patient who wishes to enroll in the MOLST program. A Standard DNR order can be obtained from a doctor, or another individual qualified to execute such a document.
Laws – R23-4.11-MOLST
Required to Sign (MOLST) – Physician/RNP/APRN/PA and patient (or representative).
How to Write
Step 1 – Download the Rhode Island MOLST form in PDF.
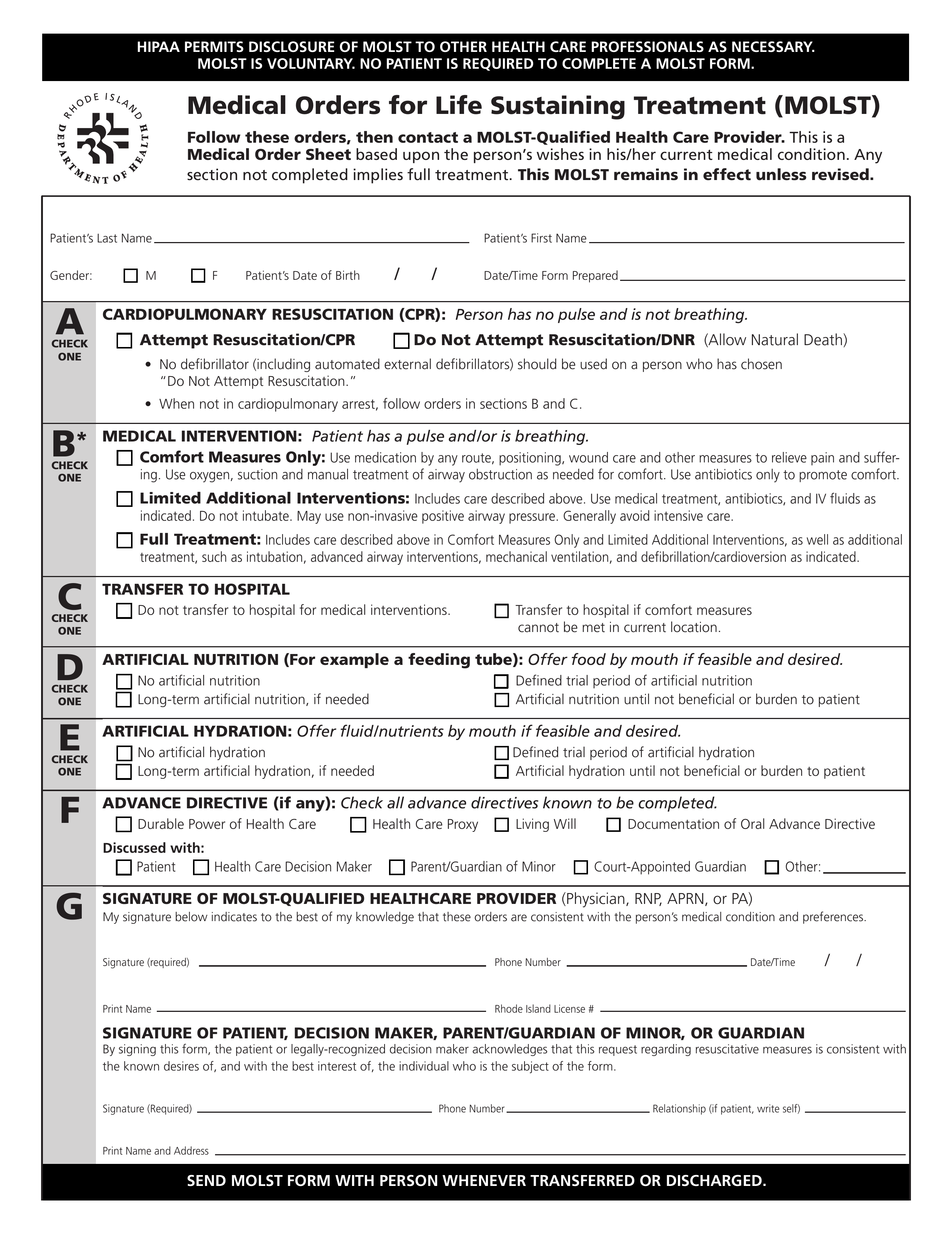
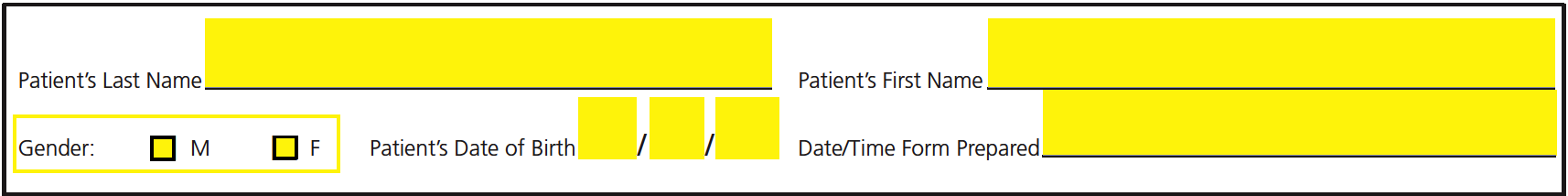
Step 2 – Use the first set of fields to specify the patient’s last name, first name, gender, date of birth, and the date/time the form was prepared.
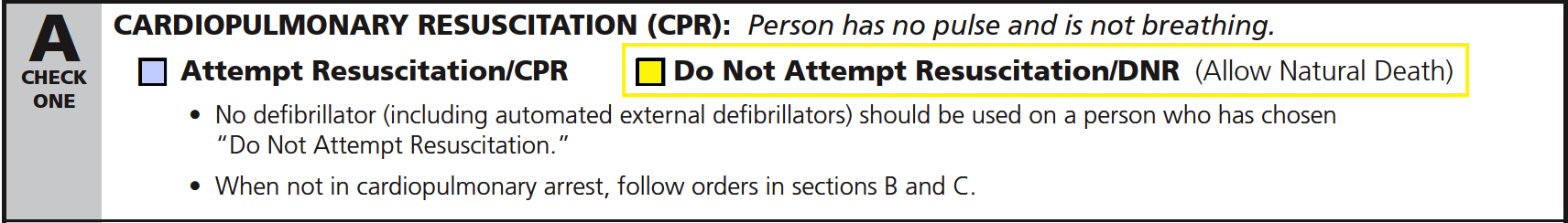
Step 3 – In section A, you will need to choose one (1) of the two (2) options to indicate whether or not the patient wishes to receive CPR when they are not breathing or have no pulse.
Choose “Attempt Resuscitation/CPR” if the patient would like to be resuscitated.
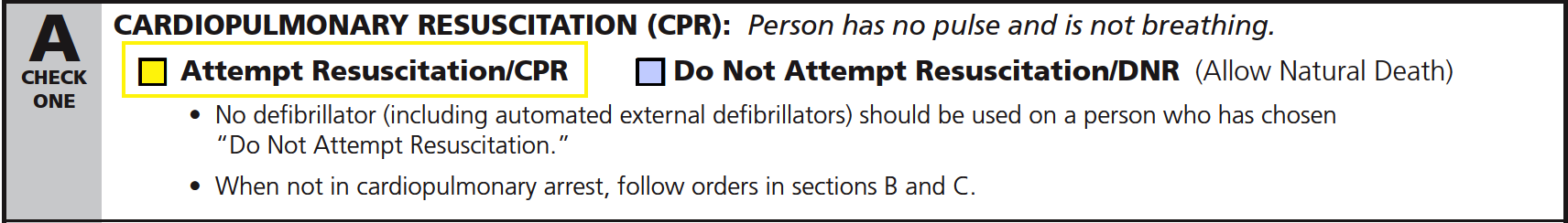
Choose “Do Not Attempt Resuscitation/DNR” if the patient does not wish to be resuscitated.
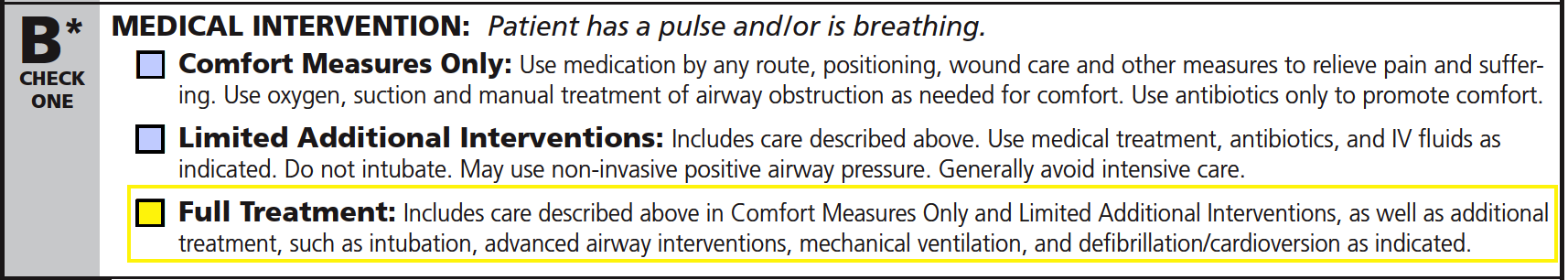
Step 4 – The medical interventions available in section B only apply when the patient has a pulse or is able to breathe. Choose one (1) of the available options to specify the treatments desired by the patient.
Select “Comfort Measures Only” if the patient would like to receive treatments to relieve pain and suffering such as suction and manual clearing of airway obstruction.
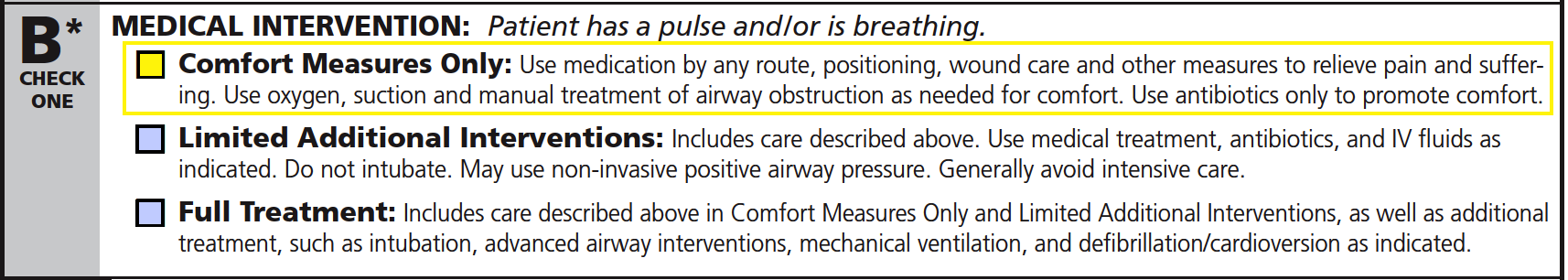
Select “Limited Additional Interventions” if the patient would like to receive the treatments offered in Comfort Measures Only as well as antibiotics, IV fluids, medical treatment, and non-invasive positive airway pressure. No intubation shall be applied, and intensive care should be avoided.
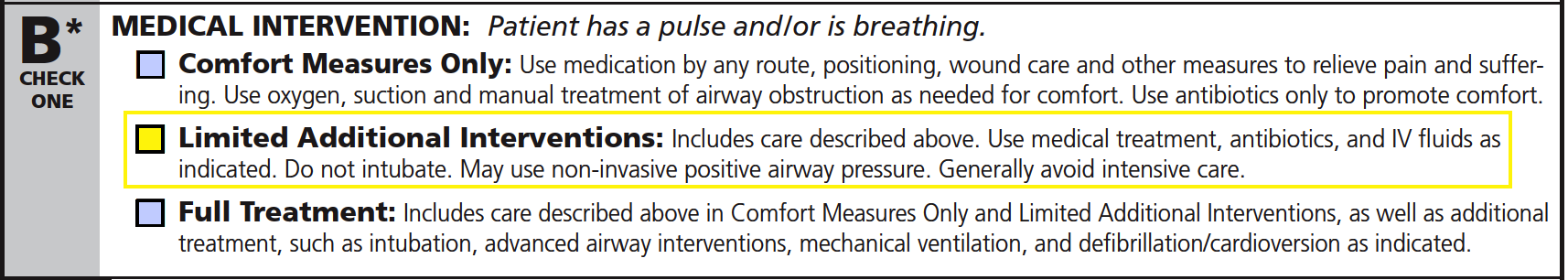
Select “Full Treatment” if the patient would like to receive the treatments described in both Comfort Measures Only and Limited Additional Interventions. This option includes additional treatments such as advanced airway interventions, intubation, mechanical ventilation, and defibrillation/cardioversion.
Step 5 – Select one (1) of the boxes in section C to indicate whether or not the patient should be transferred to a hospital for medical interventions. Select the option on the left if the patient should not be moved to a hospital. If the patient should be transferred to the hospital when their comfort measures cannot be met at their current location, select the option on the right.
![]()
Step 6 – Check one (1) of the boxes in section D to specify the desired method of artificial nutrition (if any). The available options are as follows:
- No artificial nutrition
- Defined trial period of artificial nutrition
- Long-term artificial nutrition (if needed)
- Artificial nutrition until not beneficial or burden to patient
![]()
Step 7 – Section E is used to indicate the preferred method of artificial hydration (i.e., fluids/nutrients). Select one (1) of the following options to specify which artificial hydration method shall be used:
- No artificial hydration
- Defined trial period
- Long-term (if needed)
- Artificial hydration until not beneficial or burden to patient
![]()
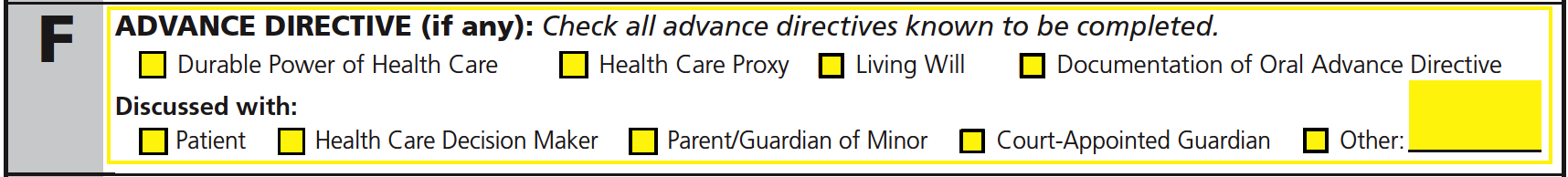
Step 8 – In section F, check any of the first four (4) checkboxes to indicate the advance directives which are known to be completed (if any). Next, below “Discussed with,” choose one (1) of the boxes to specify who requested the MOLST form (if other, explain).
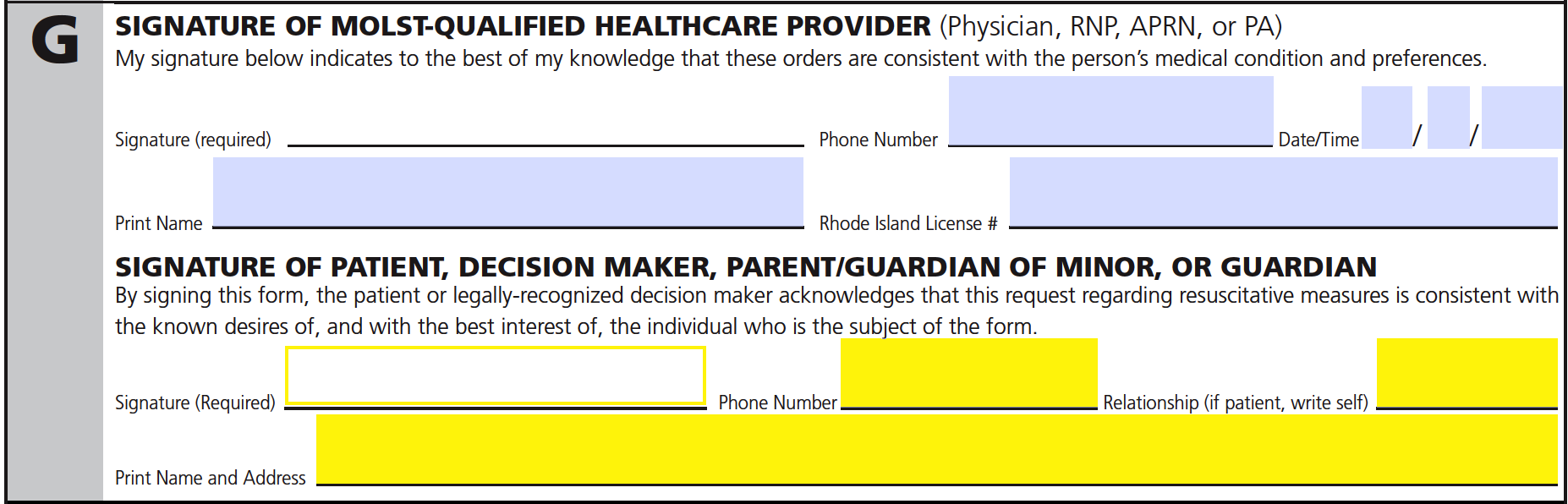
Step 9 – The first portion of section G must be completed by the health care provider authorized to handle the MOLST form (physician, RNP, APRN, or PA). The individual must provide their signature, phone number, printed name, Rhode Island license number, and enter the date/time the form was signed.
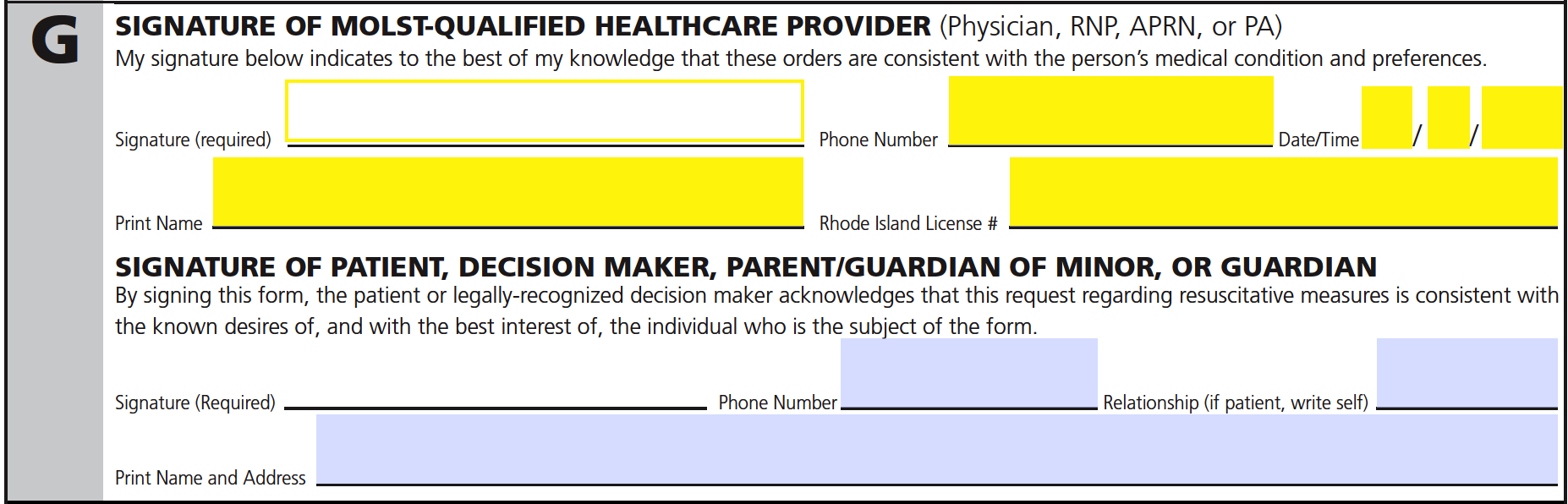
Step 10 – In the remaining spaces of section G, the patient (or qualified representative) must supply their signature, phone number, printed name, address, and describe their relationship to the patient.
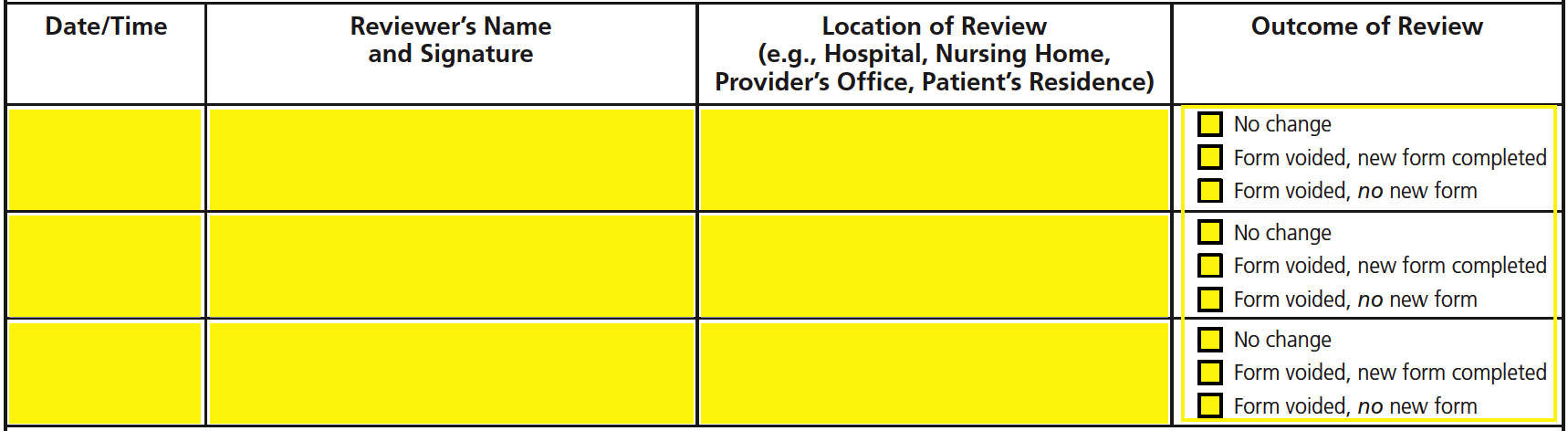
Step 11 – The remaining spaces available on page 2 of the MOLST form should only be completed by a qualified health care provider under either of the following circumstances:
- If the patient is moved to another location for treatment
- If the patient has a drastic change in their health status
- If the patient (or representative) changes their mind about the requested treatments
When any of the above circumstances apply, the qualified health care provider will be required to review the MOLST form and supply the following information in the available fields:
- Date/time
- Signature
- Location of review
- Outcome of review