Updated April 04, 2024
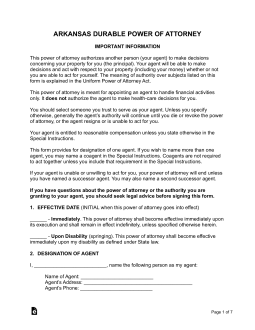
An Arkansas advance directive allows a person to articulate their preferences for medical treatment and choose someone to make health care decisions on their behalf. The form is used as a guide for a hospital on how to treat someone in the chance they should become permanently incapacitated with no possible cure. For these reasons, it is common for elderly individuals or people with severe health issues.
Advance Directive Includes
Table of Contents |
Laws
Statutes – § 20-6-101 to § 20-6-117 (Arkansas Healthcare Decisions Act)[1]
Signing Requirements – Two witnesses or a notary public.[2]
Versions (2)
Download: PDF
Download: PDF
How to Write
Download: PDF
Arkansas Advance Directive
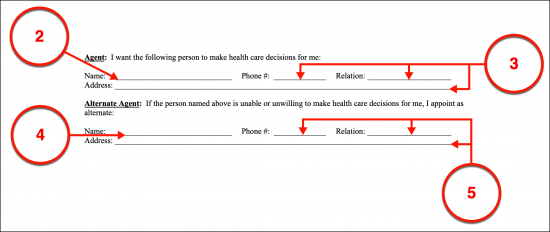
(1) Arkansas Principal. The full name of the Arkansas Principal will be needed to attach this document to his or her identity as a Patient in this state. The Principal will use this paperwork to authorize a specific Party to represent his or her medical preferences if he or she has been incapacitated.
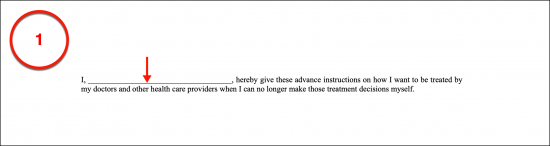
(2) Name Of Arkansas Health Care Agent. The Arkansas Health Care Agent will also need to be attached by name to this document. The Arkansas Health Care Agent will take on the responsibility of conferring with Arkansas Physicians regarding the Patient’s care when that Patient is not able to communicate in a comprehensible manner.
(3) Arkansas Health Care Agent Information.
(4) Alternate Arkansas Health Care Agent. After the Arkansas Patient’s Health Care Representative has been identified, it will be time to engage a precaution offered through this document. To ensure the Principal’s representation is consistent, an Alternate Arkansas Agent or Successor Agent can be granted the right to represent the Patient if the original appointment does not fill this role adequately, does not wish to when called upon to do so, or lacks the ability or availability necessary to represent the Principal. The Alternate Arkansas Agent is held in reserve with no authority to represent the Patient until the original Arkansas Agent is no longer effective.
(5) Alternate Arkansas Health Care Agent Information.
Quality Of Life
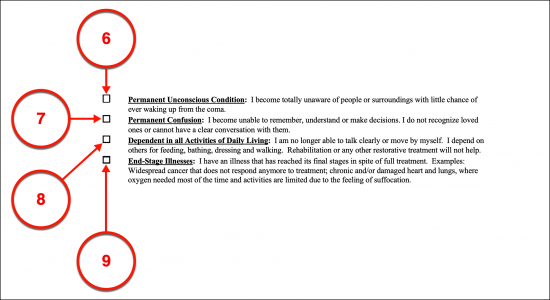
Select Item 6, Item 7, Item 8, And/Or Item 9 As Needed
(6) Permanent Unconscious Condition. Select the first statement’s checkbox to inform Arkansas Medical Professionals that the Principal issuing this paperwork does not consider being permanently unconscious to be a tolerable or acceptable way to live.
(7) Permanent Confusion. If the Principal becomes unable to recognize his or her surroundings or normally familiar people as a result of being in a state of permanent confusion or incognizance and wishes to declare this as a poor quality of life, then the second statement should be selected.
(8) Dependent In All Activities Of Daily Living. If you do not wish Arkansas Physicians to consider your quality of life acceptable when you will be dependent on other Parties for daily personal maintenance (i.e., brushing teeth, washing, eating) then check the third checkbox statement to adopt this directive.
(9) End-State Illnesses. Select the final statement to inform Arkansas Medical Personnel that being incapacitated in the final stages of a terminal illness should not be considered an acceptable quality of life for the Principal issuing this paperwork.
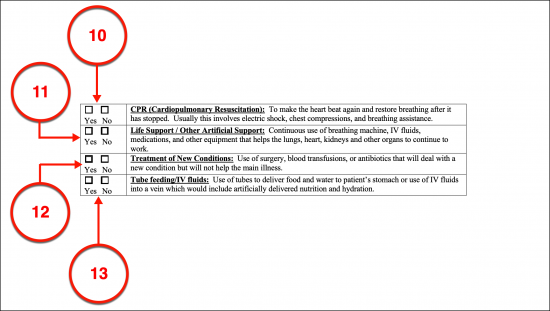
Treatment
(10) CPR (Cardiopulmonary Resuscitation). This document will also be used to inform which treatments should be withheld when the Principal is rendered incapable of communication and subjected to an unacceptable quality of life. If the Principal wishes to authorize the use of CPR even when suffering from a significant loss to the quality of life, then the “Yes” box must be selected in the first statement. Otherwise, for the Principal to prematurely refuse CPR or cardiopulmonary resuscitation when enduring an unacceptable quality of life then the first checkbox in the provided list of treatments must be selected.
(11) Life Support/Other Artificial Support. The Principal’s directives can include consent or refusal for life support measures to be implemented when he or she is subjected to an intolerable quality of life with the selection of the appropriate checkbox (“Yes” or “No”) presented with the second statement.
(12) Treatment Of New Conditions. The Principal can also dispense his or her consent or denial to procedures needed to treat only new medical conditions that arise when he or she is suffering an intolerable quality of life (i.e., becoming diabetic while in a coma).
(13) Tube Feeding/IV Fluids. Artificially administered food and water when the Principal has an unacceptable quality of life and cannot intake nutrients and/or liquids can be approved or refused with the “Yes” or “No” checkbox, respectively.
Durable Power Of Attorney For Health Care
(14) Arkansas Principal. The Durable Power Of Attorney allows the Principal to name a Health Care Attorney-in-Fact to handle his or her treatment decision. The power to represent the Principal in this manner must be given by the same Principal thus, begin this document by supplying the full name of the Principal to the title.

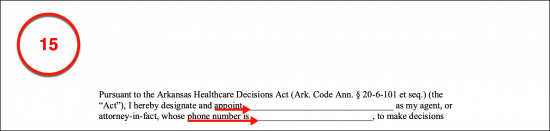
(15) Medical Attorney-in-Fact Name And Phone Number. Present the full name and contact telephone number of the Attorney-in-Fact who is meant to convert the Principal’s preferences to Arkansas Medical Professional.
Successor Agent Designation.
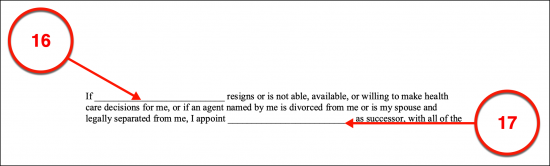
(16) Confirm The Medical Attorney-in-Fact’s Name.
(17) Successor Agent. If the Medical Attorney-in-fact named in this role is unable, disqualified, or unwilling to function in this role then the Principal can be left vulnerable and without his or her medical directives known. A Successor Agent can be set in place to take the role of the Arkansas Medical Attorney-in-Fact should this role become abandoned or vacant. Until then, the Successor will not have any authority to represent the Principal. If a Private Party that the Principal trusts and approves of will be held in reserve so that he or she can automatically be appointed as the Principal’s Medical Attorney-in-Fact in Arkansas upon the vacancy of this role, then record the Successor’s full name where it is requested.
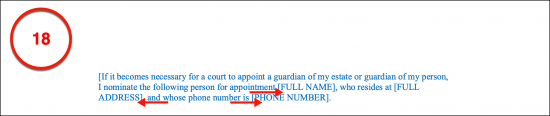
(18) Nomination Of Arkansas Court-Appointed Guardian. If the Principal has decided to nominate a Party to be appointed as an Arkansas Court-Appointed Guardian or Conservator, in case Arkansas Courts decide this is necessary, then the Principal’s Nomination must be identified by name with his or her address and phone number. This is not a mandatory action for this form and it should be noted that Arkansas Courts are not obligated to accept the Principal’s Nominee for the position.
Signature Execution
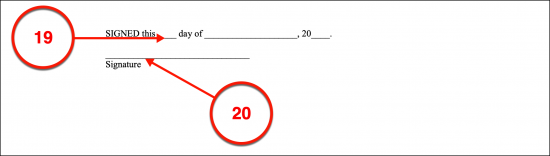
(19) Signature Date. The exact date that the Principal signs this document must be established through his or her direct report.
(20) Principal Signature. Immediately after recording the date, the Principal must sign this document then release it to the first Party who will verify his or her act of signing.
Witness Verification
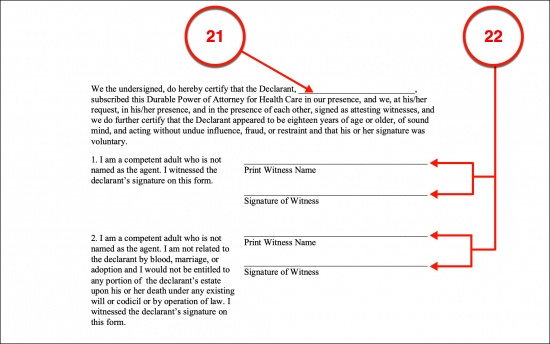
(21) Preparing the Witness Statement. The printed name of the Principal must be used to apply the Witness’s declaration properly.
(22) Witness Signatures. Each Witness will be expected to print and sign his or her name to acknowledge the statement regarding the authenticity of the Arkansas Principal’s signing. Two Witnesses will be needed for this function thus, two unique signature areas have been provided to accommodate each testimonial signature.
Notary Acknowledgment
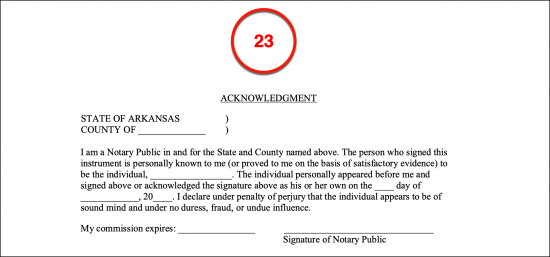
(23) Notarization. The Arkansas notarization process can only be conducted by a licensed Notary Public. A distinct section has been provided for this reason.
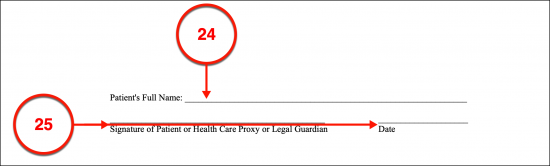
Do Not Resuscitate Order
(24) Patient’s Full Name. The Arkansas Patient or Declarant can also issue a Do Not Resuscitate Order under the supervision of a licensed Physician, Physician Assistant, or APR Nurse. This will inform Arkansas Responders that the Arkansas Patient or Declarant does not wish CPR used to revive him or her when he or she is found with a nonfunctional heart or lungs. If the Arkansas Patient or Declarant wishes to make this statement, then his or her full name must be presented in print where requested.
(25) Arkansas Patient Signature And Date. The Arkansas Patient or Declarant must sign his or her name and report the current date to prove his or her intent to issue this DNR.
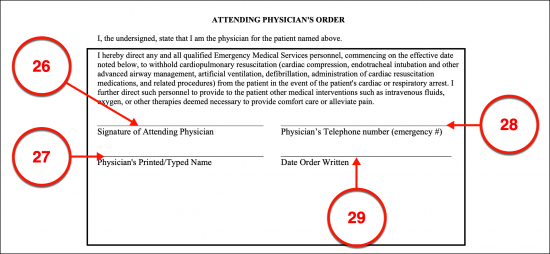
Attending Physician’s Order
(26) Signature Of Attending Physician. As mentioned, the licensed Physician, Physician’s Assistant, or APR Nurse must participate in the issuing of this paperwork. This Medical Professional must sign his or her name to acknowledge this Patient’s DNR.
(27) Physician’s Printed/Typed Name.
(28) Physician’s Telephone Number.
(29) Date Order Written. The calendar date when the Physician signs this paperwork is required.
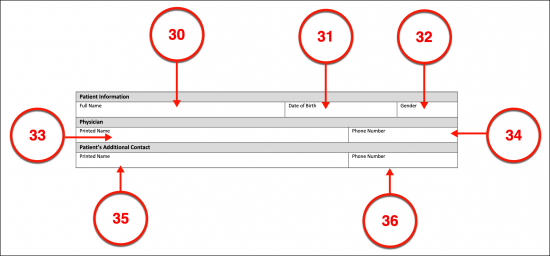
Arkansas POLST
(30) Arkansas Patient Name. An institutional method for attaching the Arkansas Patient or Declarant’s medical directives is the Arkansas MOLST which sets these instructions to paper under a qualified Medical Provider’s supervision. This record is then set in the Patient’s medical files for future reference by Arkansas Medical Responders and Personnel. Naturally, the full name of the Arkansas Patient or Declarant will need to be presented at the beginning of this paperwork.
(31) Date Of Birth. Some additional information will be needed to present the Arkansas Patient’s identity beginning with his or her birth date.
(32) Gender
(33) Physician Printed Name. The licensed Physician aiding the Patient with this form must be identified as well. His or her printed name and professional phone number are required.
(34) Phone Number.
(35) Patient’s Additional Contact. The full name of the Arkansas Patient or Declarant’s Emergency Contact should be included with this report. This can be a trusted Family Member or Medical Attorney-in-Fact that the Arkansas Patient wishes contacted if he or she is found unable to communicate and enduring a severe medical event.
(36) Arkansas Patient Contact Phone Number.
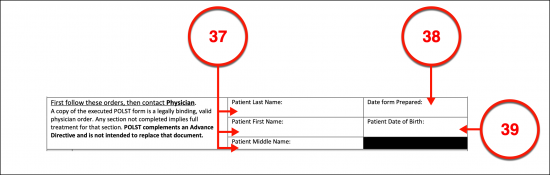
POLST
(37) Arkansas Patient’s Full Name. The Arkansas POLST will require the Patient’s name recorded in a standard filing format (i.e., last, first, and middle name).
(38) Preparation Date. The calendar date when this form is prepared must be documented.
(39) Arkansas Patient Date Of Birth.
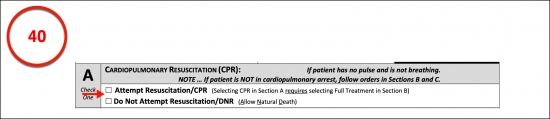
A. Cardiopulmonary Resuscitation (CPR)
(40) Declarant’s CPR Directive. The decision to accept cardiopulmonary resuscitation when the Arkansas Patient requires intervention because his or her heart and lungs no longer function can be issued with a selection of the statement of consent or that of refusal from the first section.
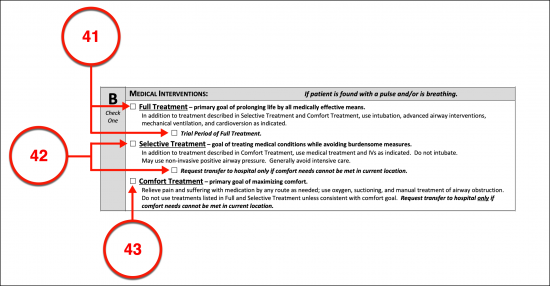
B. Medical Interventions
Choose Item 41 Or Item 42 Or Item 43
(41) Full Treatment In Arkansas. The efforts of attending Arkansas Medical Responders can be set by the Patient or Declarant through this form. That is if the Patient authorizes Arkansas Health Providers to provide the full medical treatment needed and available to maintain the Declarant’s life, then the checkbox requesting Full Treatment should be selected. An additional option for this declaration allows the Arkansas Patient to approve full treatment only for a trial period.
(42) Selective Treatment. The Arkansas Declarant can use this section of the MOLST to instruct Physicians that he or she only approves of treatment that balances treatment with comfort care as the goal. This will allow a limited amount of intervention that will inform Physicians that treatments should exclude invasive procedures such as intubation. This option will also allow the Principal to declare it should be used for only a limited amount of time.
(43) Comfort Treatment. The Arkansas Patient can issue a declaration that he or she intends to refuse all treatment unless its goal is comfort care and that a trip to the hospital can only be made if this is needed to keep him or her comfortable and pain-free.
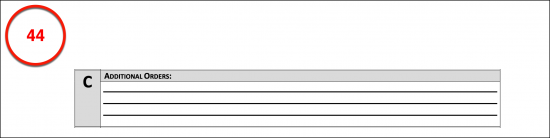
C. Additional Orders
(44) Patient Directives. The Arkansas Patient or Declarant can deliver specific instructions regarding topics such as how long a trial period should be or the use of specific treatments that have thus far been left unmentioned.
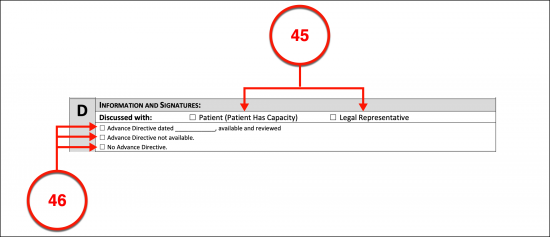
D. Information And Signatures
(45) Source Of Information. The discussion that results from this document must be defined. By selecting the appropriate checkbox, the Physician can indicate if he or she worked directly with the Arkansas Patient or with a Proxy or Legal Representative of the Arkansas Patient.
(46) Advance Directive Status. If the Arkansas Physician has reviewed the Patient’s advanced directive, then he or she should indicate this fact by choosing the correct check box and providing the date the review occurred. Otherwise, the Physician should indicate that the Arkansas Patient’s is not available or that no such document has been issued.
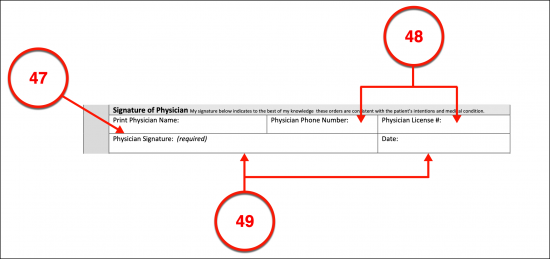
Signature Of Physician
(47) Physician’s Printed Name.
(48) Physician’s Supporting Information. The Arkansas Physician’s telephone number and Physician’s License number must be submitted.
(49) Arkansas Physician Signature And Date. The Arkansas Physician completing this document must deliver his or her approval to the Arkansas Patient or Declarant’s directives by signing it then entering the current calendar date.
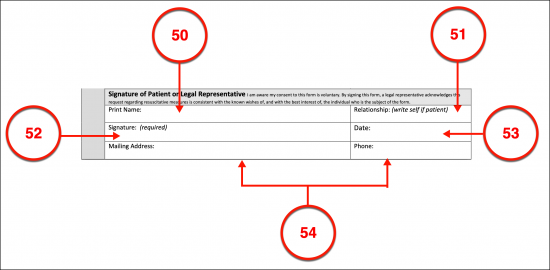
Signature Of Patient Of Legal Representative
(50) Arkansas Declarant’s Printed Name. It is crucial that this document demonstrates that it is an accurate representation of the Arkansas Patient’s directives. This requires a signature process to be completed by the Arkansas Declarant or his or her Legal Representative (i.e., Medical Attorney-in-Fact, Health Care Agent, Court Appointed Guardian, etc.). The Printed name of the person who will sign this document must be presented.
(51) Relationship With Signature Party. If the Arkansas Patient is signing on his or her own behalf then he or she should define this relationship as “Self,” otherwise the relationship the Arkansas Signature Declarant holds with the Patient being discussed should be documented.
(52) Arkansas Declarant’s Act Of Signing. The Arkansas Patient (or his or her Legal Representative) must sign this document.
(53) Signature Date.
(54) Arkansas Patient’s Contact Information. The mailing address and telephone number where the Arkansas Patient or Signature Representative should be reported.
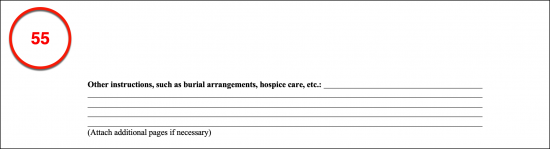
Other Instructions
(55) Additional Arkansas Patient Directives. Present all additional provisions concerning items such as the Patient’s preferred hospice care programs, burial preferences, or requested experimental treatments if they should be included with the declarations made through the MOLST.
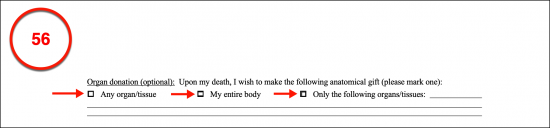
(56) Organ Donation Status. The Arkansas Patient can declare that he or she wishes to make an anatomical gift of any organ or tissue needed upon his or her death, his or her entire body, or a specific list of body parts that are defined in the final area.
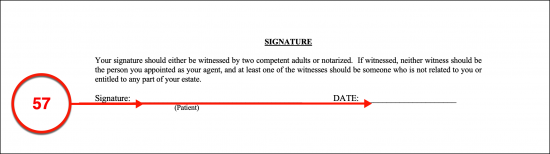
Signature
(57) Patient Signature And Date. The Arkansas Declarant must sign the MOLST’s near-death requests and submit the current date.
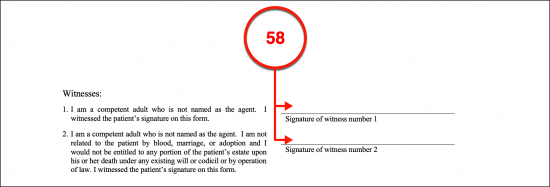
(58) Witness Signatures. Two Witnesses must watch the Arkansas Principal sign his or her name and will be required to provide signature confirmation that this order’s execution was signed by the Arkansas Principal or Authorized Legal Representative.
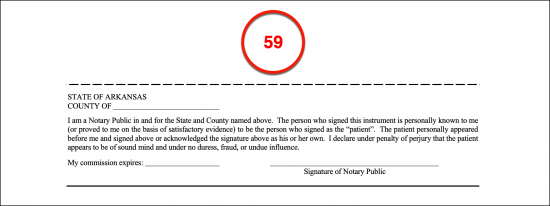
(59) Notary Verification. The Arkansas Notary Public obtained to notarize the Patient’s signing will provide his or her credentials after completing the notarization area.
Related Forms
 Durable (Financial) Power of Attorney
Durable (Financial) Power of Attorney
Download: PDF, MS Word, OpenDocument
Download: PDF, MS Word, OpenDocument