Updated June 02, 2022
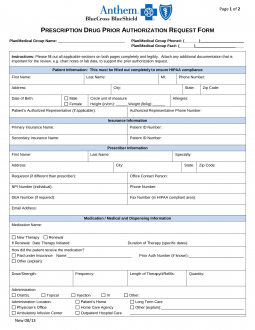
An Anthem (Blue Cross Blue Shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost. The form contains important information regarding the patient’s medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patient’s health care plan. Anthem has also made available a series of forms for specific medications which may provide more efficient service when making a request.
How to Write
Step 1 – At the top of the form, supply the plan/medical group name, plan/medical group phone number, and plan/medical group fax number.
Step 2 – In “Patient Information”, provide the patient’s full name, phone number, full address, date of birth, sex (m/f), height, and weight. Also, specify any allergies and give the name and phone number of the patient’s authorized representative (if applicable).
Step 3 – In “Insurance Information”, provide the primary and secondary insurance providers along with the corresponding patient ID numbers.
Step 4 – In “Prescriber Information”, specify the prescriber’s full name, speciality, and full address. Below that, write the name of the requester (if different than the prescriber) and supply the prescriber’s NPI number and DEA number. Lastly, give the name of an office contact person along with the corresponding phone number, fax number, and email address.
Step 5 – In “Medication / Medical and Dispensing Information”, specify the medication name and indicate whether or not the request is a new therapy or a renewal (if renewal, specify the date therapy started and the duration).
Step 6 – In “Medication / Medical and Dispensing Information”, describe how the patient paid for their medication (include the insurance name and prior authorization number).
Step 7 – In “Medication / Medical and Dispensing Information”, specify the following prescription details: dose/strength, frequency, length of therapy/number of refills, and quantity.
Step 8 – In “Medication / Medical and Dispensing Information”, indicate the administration method and administration location.
Step 9 – At the top of page 2, provide the patient’s name and ID number.
Step 10 – On page 2 (1), select yes or no to indicate whether the patient has tried other medications for their condition. If yes, provide the medication name, dosage, duration of therapy, and outcome.
Step 11 – On page 2 (2), list all diagnoses and provide the ICD-9/ICD-10.
Step 12 – On page 2 (3), provide any details supporting the request (symptoms, clinic notes, lab results, etc.).
Step 13 – The prescriber must provide their signature at the bottom of the form and the date of signing.