Updated June 02, 2022
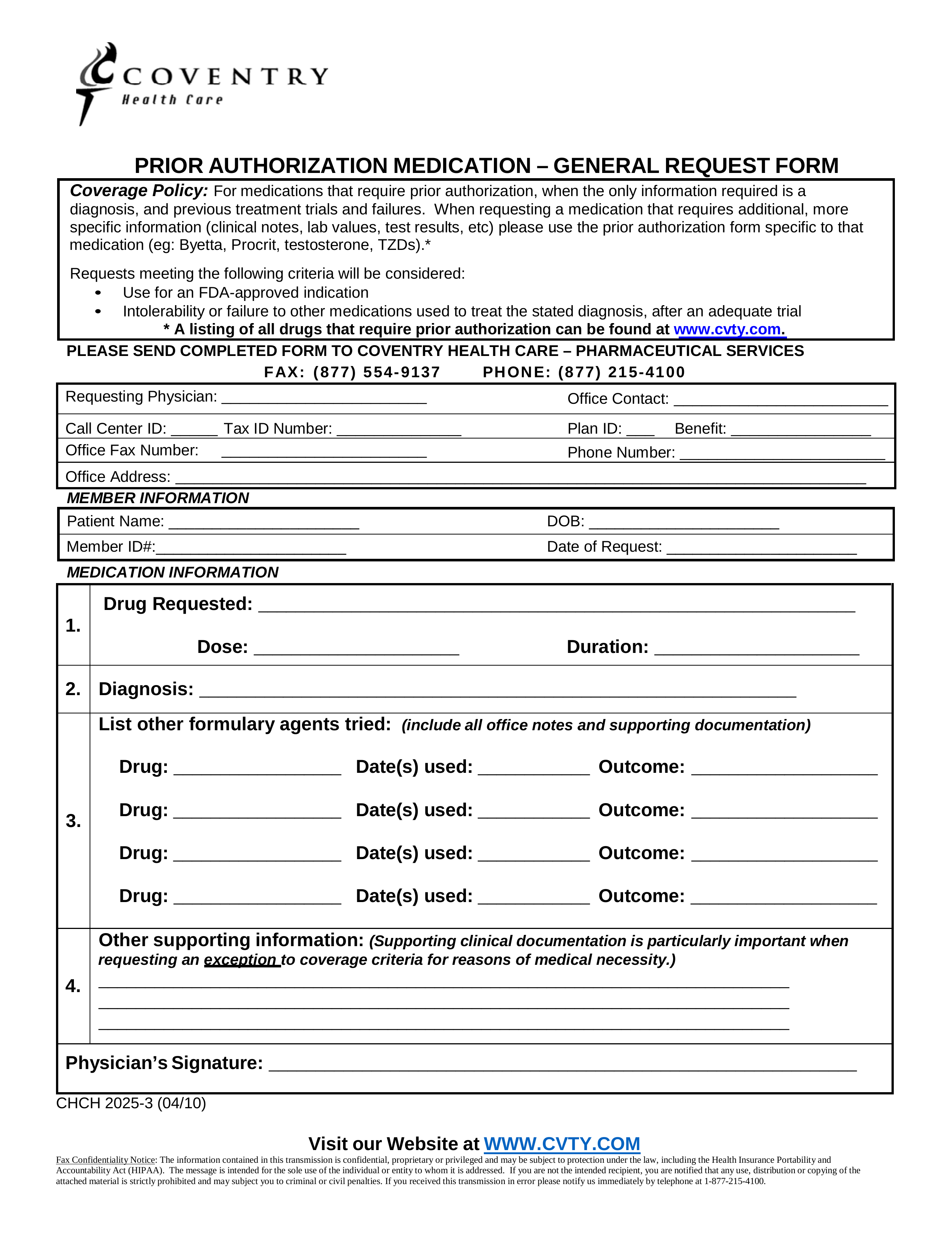
A Coventry Health Care prior authorization form is used to to verify that a patient’s health insurance plan will in fact cover the cost of a prescription. Individuals enrolled in one of Coventry Health Care’s (CHC) insurance plans will often need their prescriptions approved by CHC before medical coverage can be given. This form is a general request form; medications requiring additional information (test results, clinical notes, etc.) will require a form specific to that medication. See what medications are covered by CHC by visiting their website.
- Fax: 1 (877) 554-9137
- Phone: 1 (877) 215-4100
How to Write
Step 1 – In the first set of fields, fill in the following information related to the medical office: name of requesting physician, name of office, call center ID, tax ID number, plan ID number, benefit, office fax number, phone number, office address.
Step 2 – In “Member Information”, provide the patient’s name, date of birth, member ID number, and the date of request.
Step 3 – In “Medical Information (1)”, specify the name of the requested drug, dosage, and duration.
Step 4 – In “Medical Information (2)”, specify the diagnosis.
Step 5 – In “Medical Information (3)”, list all other formulary agents tried (drug, date(s) used, and the outcome).
Step 6 – In “Medical Information (4)”, provide any information to support the request.
Step 7 – The physician’s signature is required in the last available field.