Updated July 27, 2023
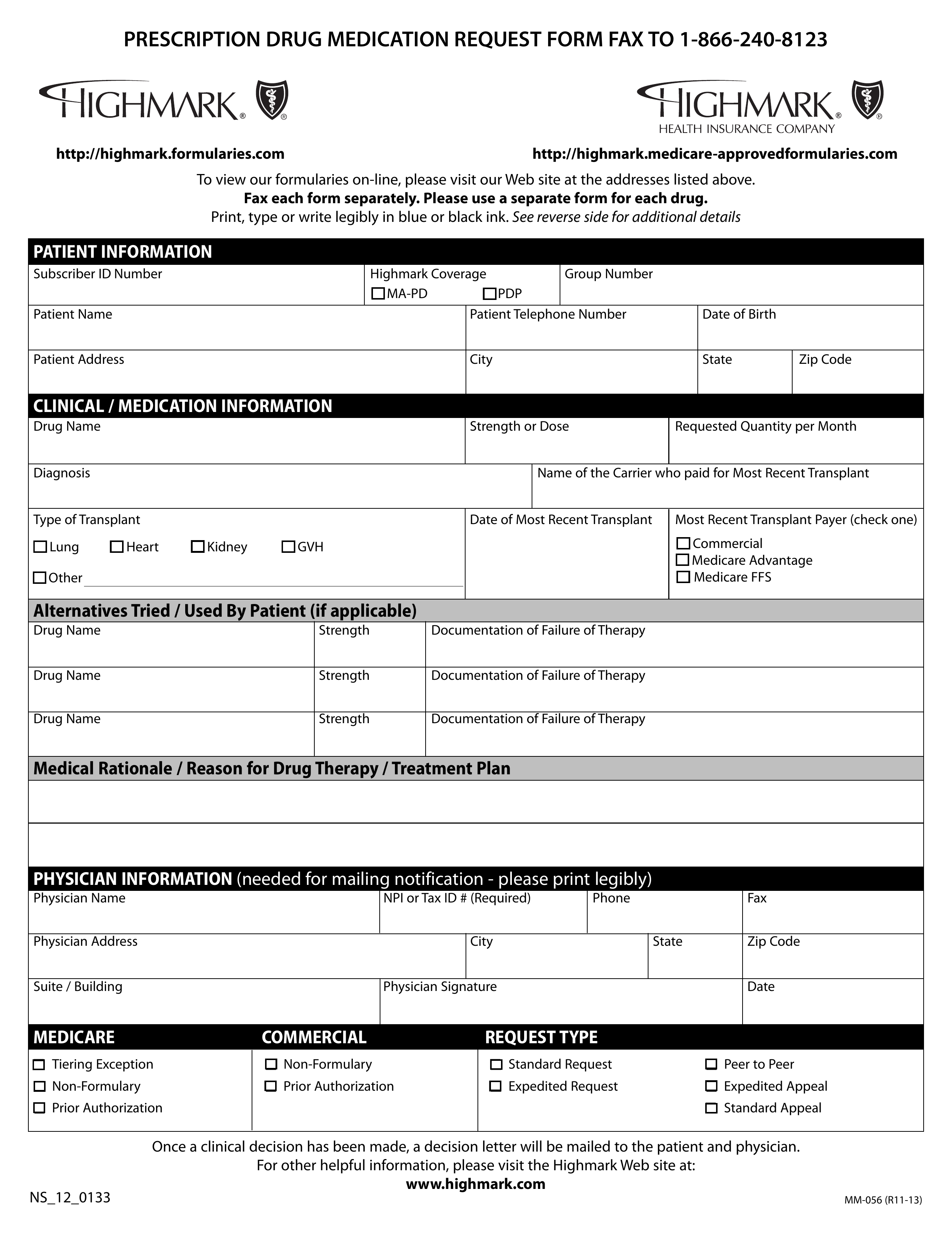
A Highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their Highmark health insurance plan. A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription. Once the form is complete, send it by fax or mail to the appropriate addresses below.
- Fax: 1 (866) 240-8123
- Mail: Medical Management & Policy, 120 Fifth Avenue, MC P4207, Pittsburgh, PA 15222