Updated July 27, 2023
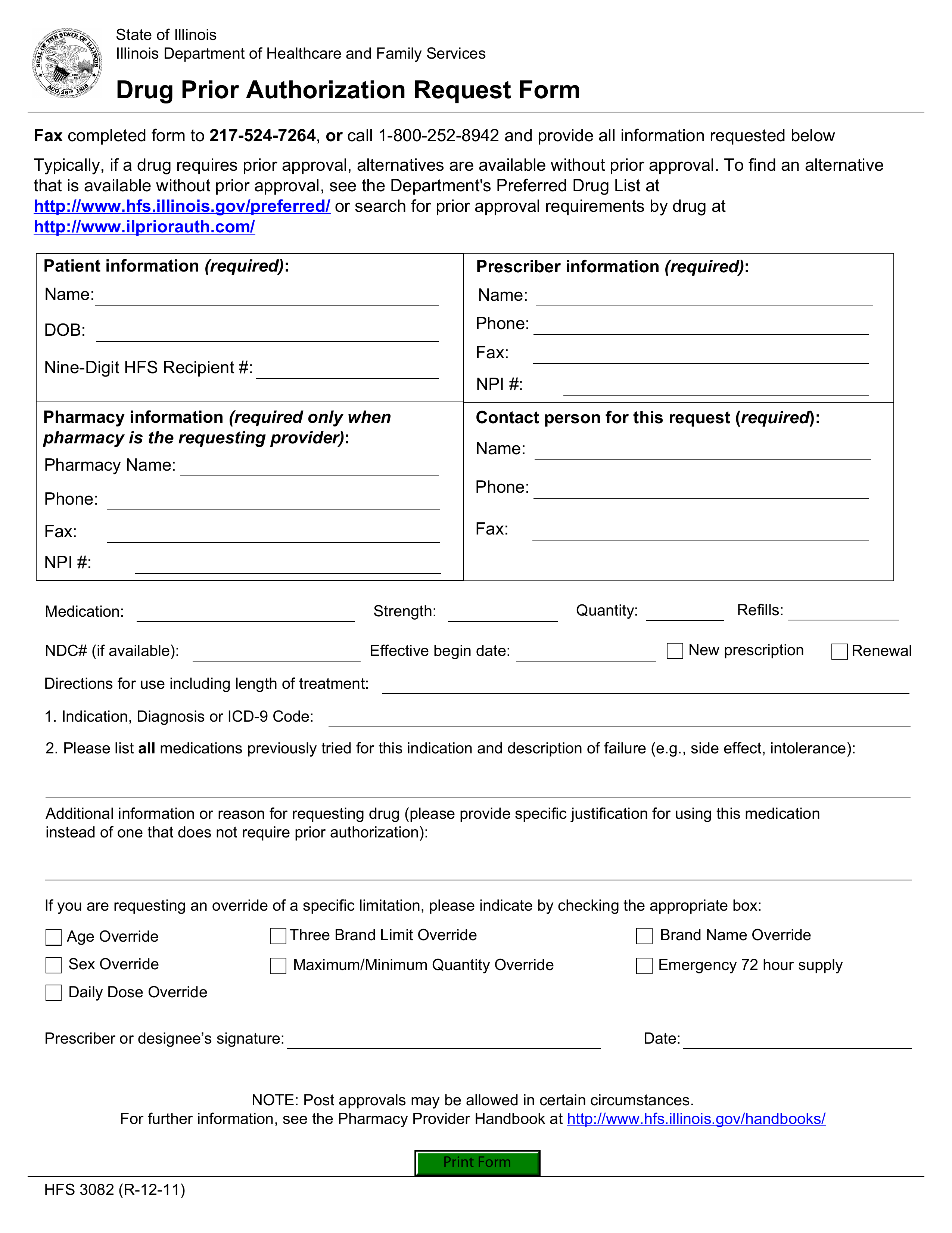
An Illinois Medicaid prior authorization form requests Medicaid coverage for a non-preferred drug in the State of Illinois. In your request, you will be asked to provide all information relevant to the patient’s diagnosis and drug trials. You must be able to justify your reason for not prescribing a drug from the Preferred Drug List (PDL). Alternatively, you can call the number provided below and make your request over the phone.
Fax – 1 (217) 524-7264
Phone – 1 (800) 252-8942
Preferred Drug List – List of pre-approved drugs by the State