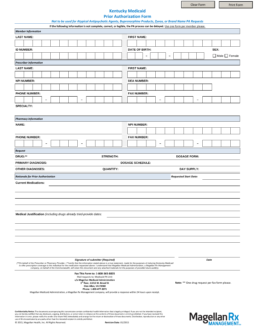
Updated July 27, 2023
A Kentucky Medicaid prior authorization form secures Medicaid coverage in the State of Kentucky for a medication that is not on the Preferred Drug List (PDL). It is intended for prescribing physicians and provides clinical justification as to why a PDL prescription can’t be used. On this page, you can download a fillable PDF version of this form to fill out, print, and submit via fax. For more information, call the Provider Relations telephone number provided below.
Phone – 1 (800) 807-1232
Fax – 1 (800) 365-8835
Preferred Drug List – List of pre-approved drugs by the State