Updated July 27, 2023
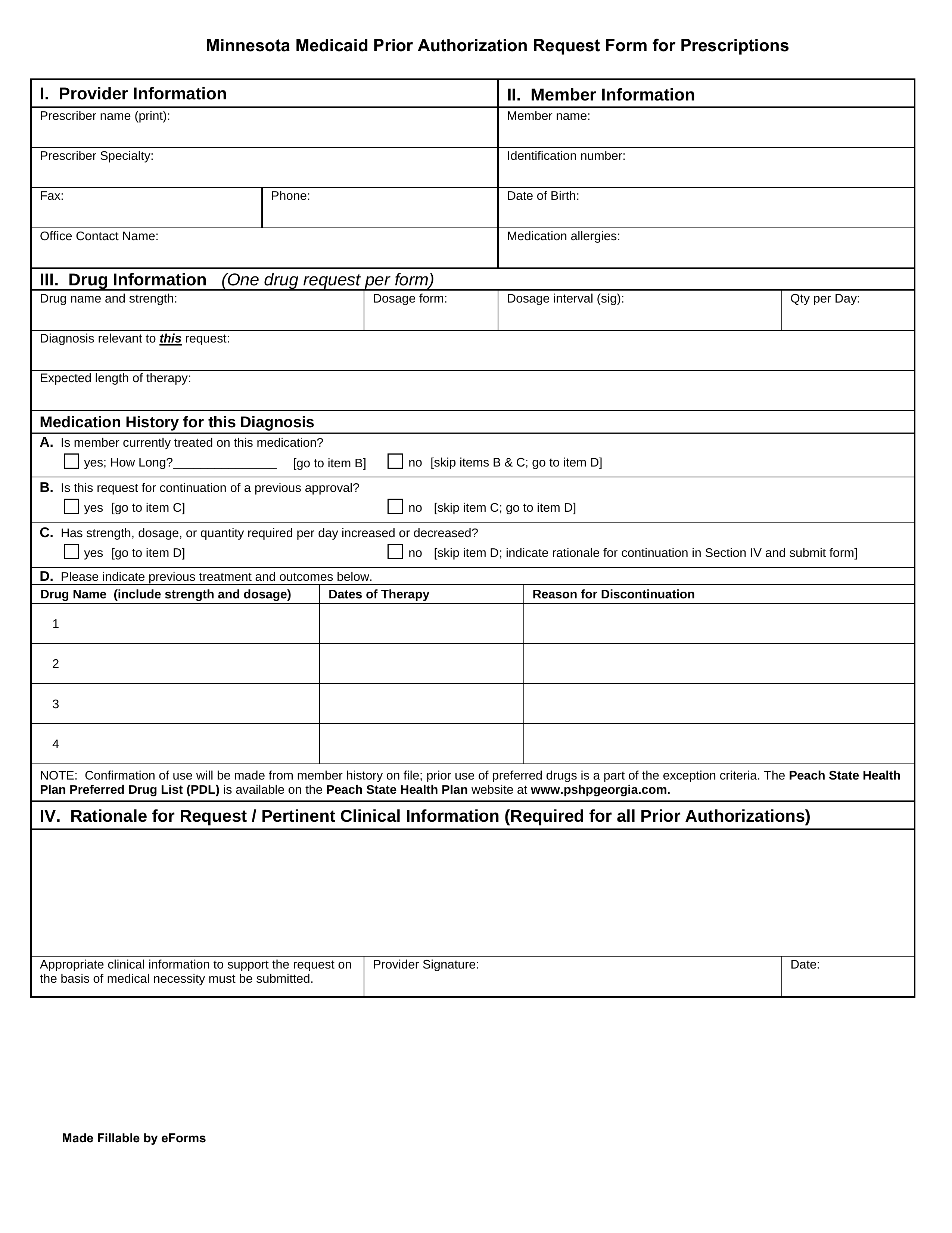
A Minnesota Medicaid prior authorization form is used when a medical professional wants to request Medicaid coverage in the State of Minnesota for a prescription that is otherwise ineligible for coverage. When submitting this form, the prescriber must include any supporting medical documentation which helps justify their request. For more information, call the phone number provided below.
Fax – 1 (866) 889-6512
Phone – 1 (866) 433-3658
Preferred Drug List – Search for pre-approved drugs online