Updated July 27, 2023
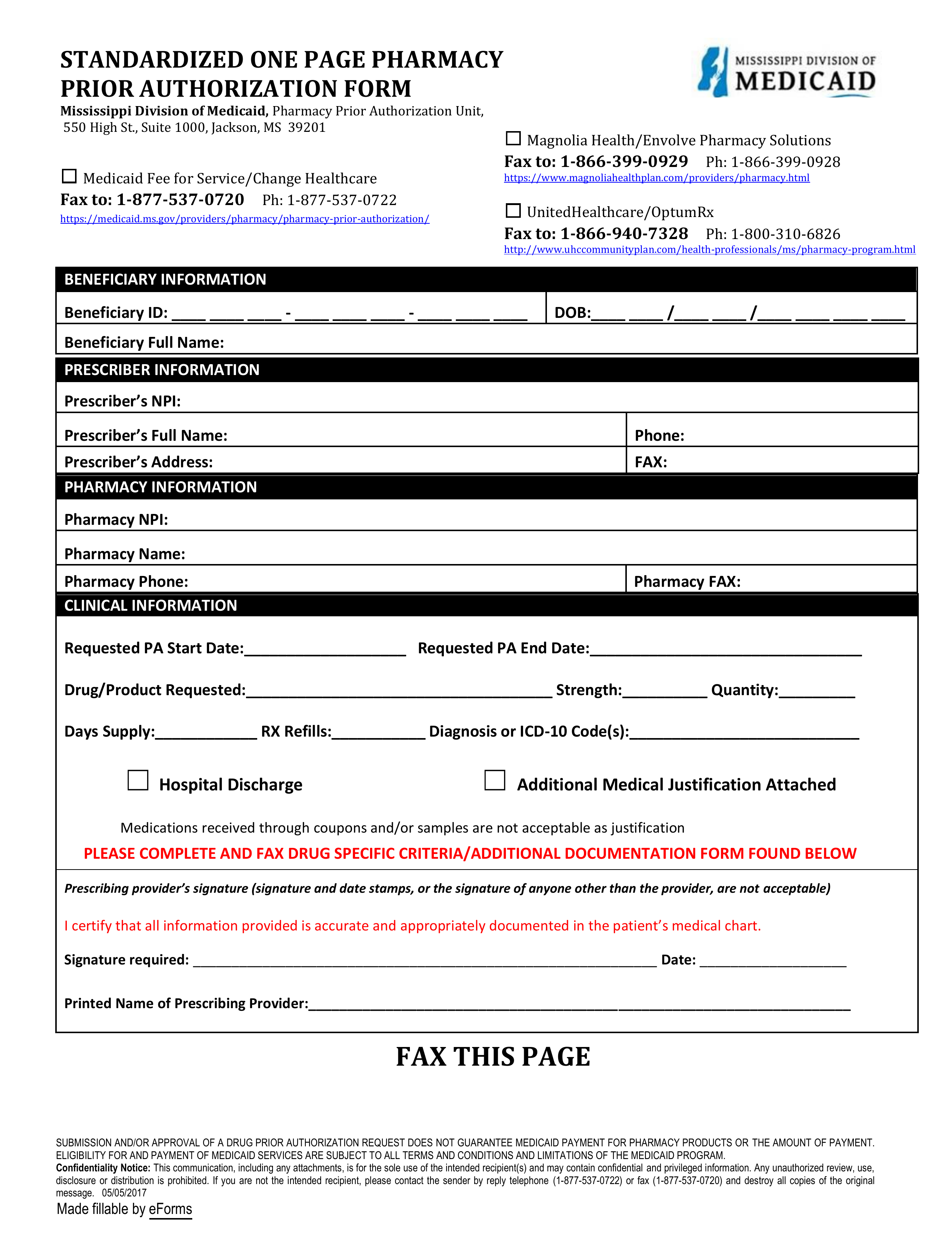
A Mississippi Medicaid prior authorization form can be completed by a prescribing physician to request a medication that is not on the state’s Preferred Drug List (PDL). Mississippi Medicaid, through the managed care program Mississippi Coordinate Access Network (MississippiCAN), covers most pharmacy services through their health care plans Magnolia and UnitedHealthCare. This request form is used to ensure that the patient in question is receiving the most appropriate and cost-effective treatment available. Once the form is submitted by the physician/medical office and reviewed by the appropriate pharmacy benefit manager (PBM), the patient will receive a statement of approval or denial of the requested drug. If approved, the patient can retrieve their prescription from the appropriate pharmacy. If the request is denied, the physician may choose to prescribe a different treatment course or submit a reconsideration form.
- Medicaid Fee-for-Service/Change Healthcare
- Fax number: 1 (877) 537-3720
- Phone number: 1 (877) 537-0722
- Magnolia Health/Envolve Pharmacy Solutions
- Fax number: 1 (866) 399-0929
- Phone number: 1 (866) 399-0928
- UnitedHealthCare/OptumRx
- Fax number: 1 (866) 940-7328
- Phone number: 1 (800) 310-6826