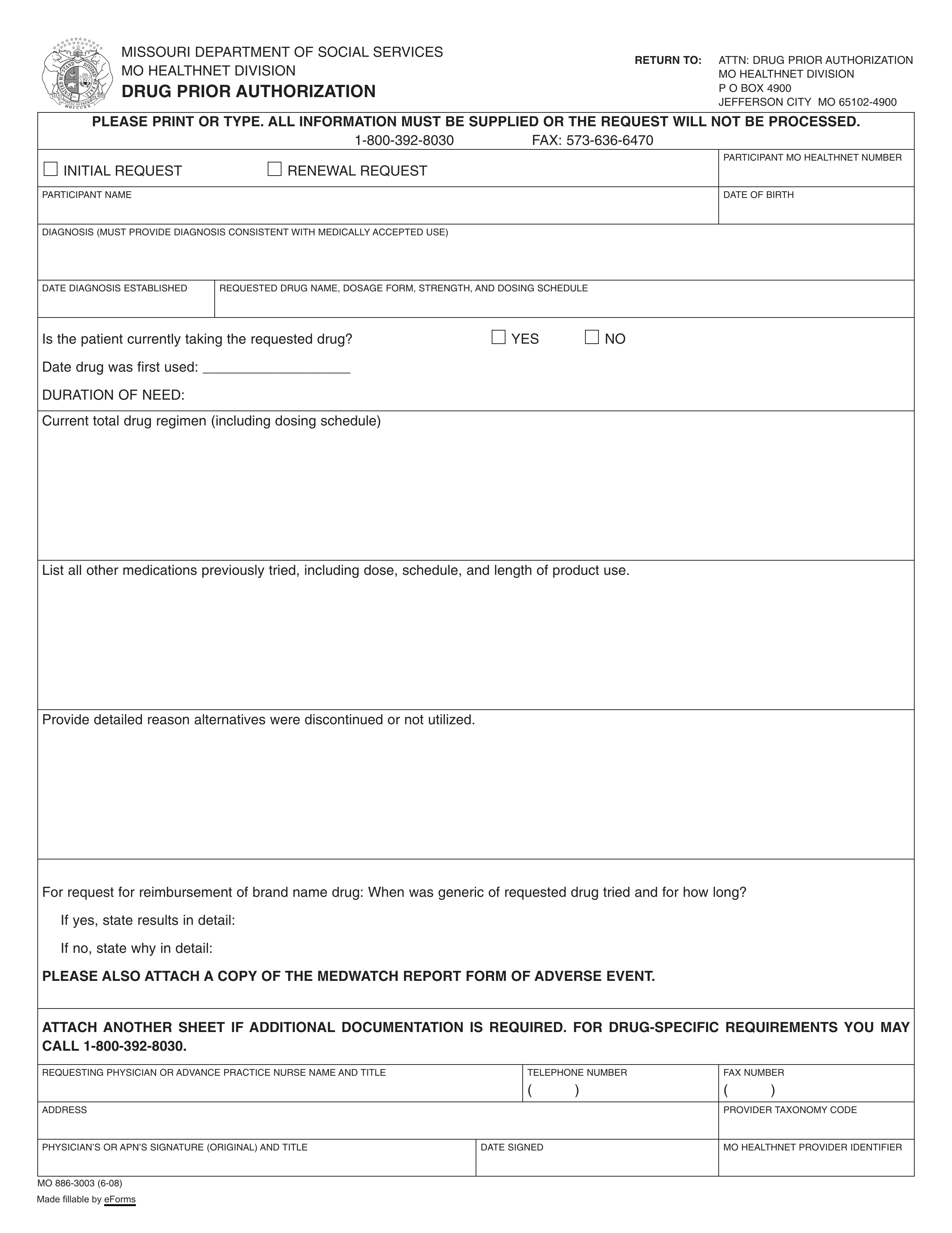
Updated July 27, 2023
A Missouri Medicaid prior authorization form is used by a prescribing medical provider to request treatment that is not covered by their patient’s state health care plan. Missouri’s Medicaid program is managed by MO HealthNet and it offers 3 plans for members to choose from: Home State Health, MissouriCare, or UnitedHealthCare. Most services, including prescription drugs, are covered by all three services, but not all medications are covered. A committee will then decide whether or not this medication is the most viable and cost-effective option for the patient.
- Department of Social Services (DSS) MO HealthNet Division phone number: 1 (800) 392-8030
- Form can be faxed to: 1 (573)636-6470
- Form can be mailed to:
ATTN: Drug Prior Authorization
MO HealthNet Division
P.O. Box 4900
Jefferson City, MO
65102-4900