Updated July 27, 2023
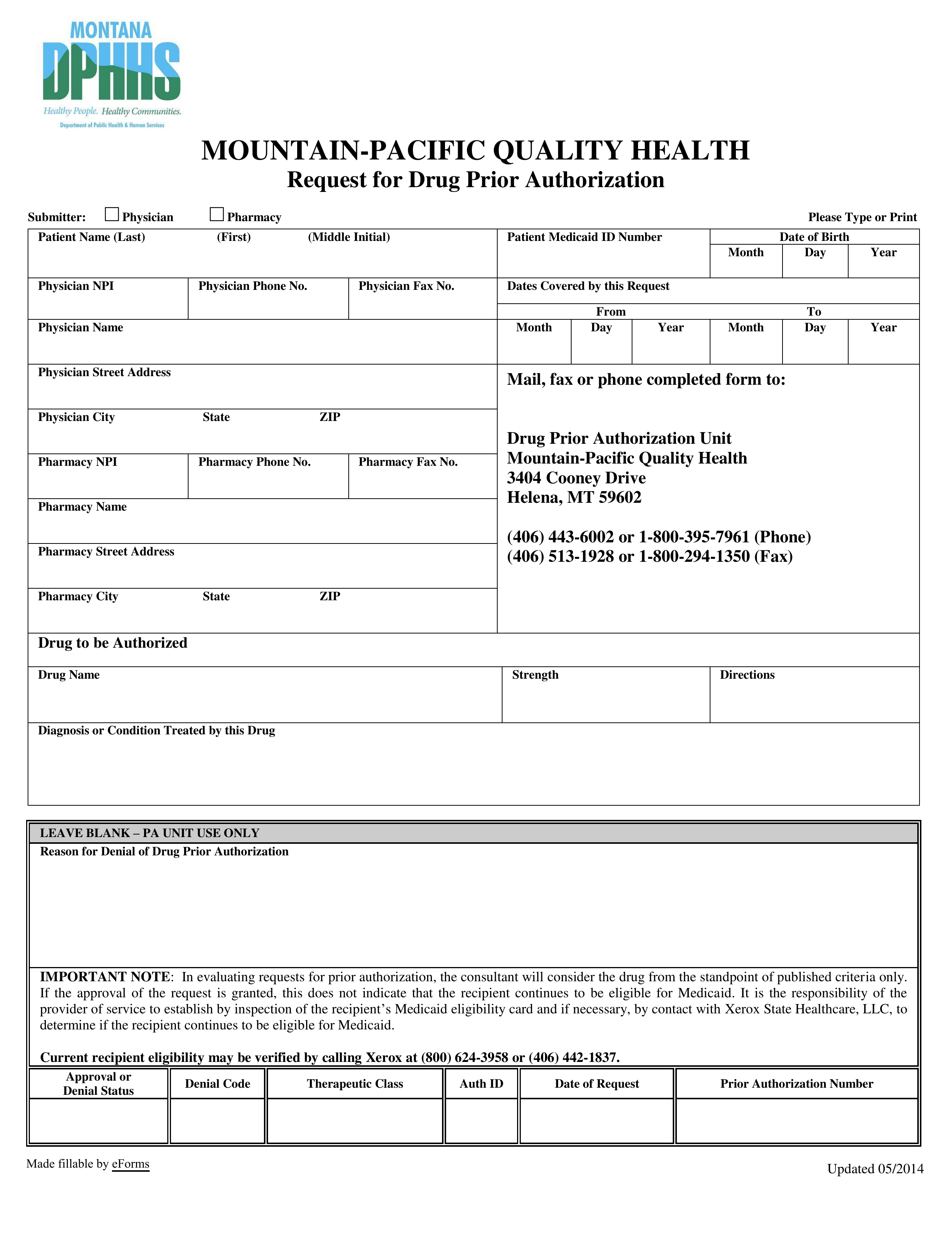
A Montana Medicaid prior authorization form is used by a physician to get permission to prescribe a drug that requires prior-authorization from Medicaid. The DPPHS provides Medicaid members with basic healthcare services, but sometimes a patient is prescribed medication that is not covered by Medicaid. The primary care case management (PCCM) program for Montana Medicaid is Passport to Health. However, Mountain-Pacific Quality Health provides Medicaid utilization review and management services for the Department of Public Health and Human Services (DPHHS) as well. Once submitted, the prior authorization form will be reviewed to ensure that the requested medication is the most appropriate and cost-effective option for the patient.
Form can be faxed to: (406) 513-1928 (Local) or 1 (800) 294-1350 (Toll-Free)
Form can be mailed to: Drug Prior Authorization Unit, Mountain-Pacific Quality Health, 3404 Cooney Drive, Helena, MT 59602