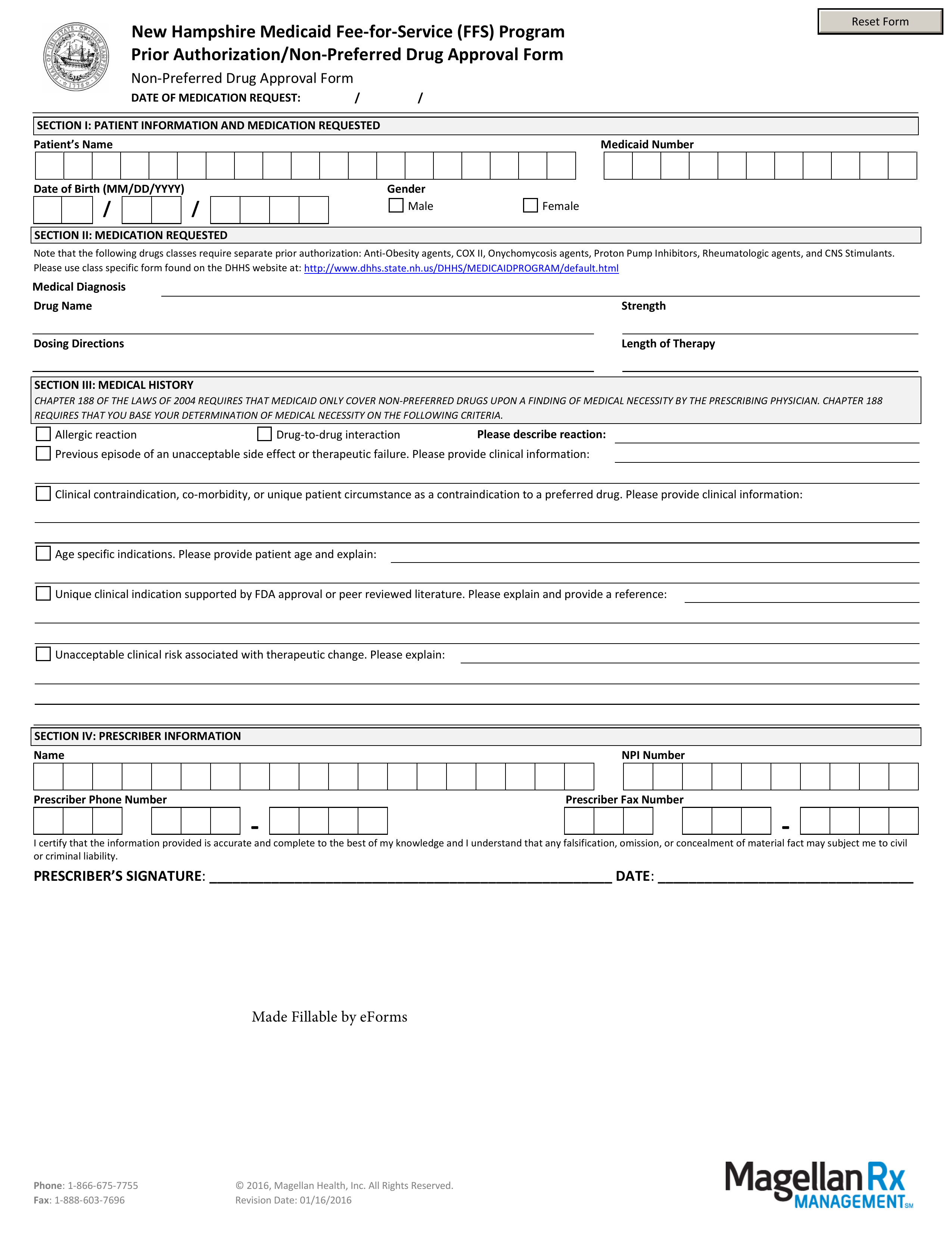
Updated July 27, 2023
A New Hampshire Medicaid prior authorization form allows a New Hampshire-based medical professional to request Medicaid coverage for a non-preferred drug. Using this form and any supporting medical documentation that you can supply, you will need to provide your clinical justification for not prescribing a drug on the Preferred Drug List (PDL). Once you have completed filling out your form, fax it along with any other attachments to the fax number provided below.
Fax – 1 (888) 603-7696
Phone – 1 (866) 675-7755
Preferred Drug List – Drugs considered preferable by the State