Updated July 27, 2023
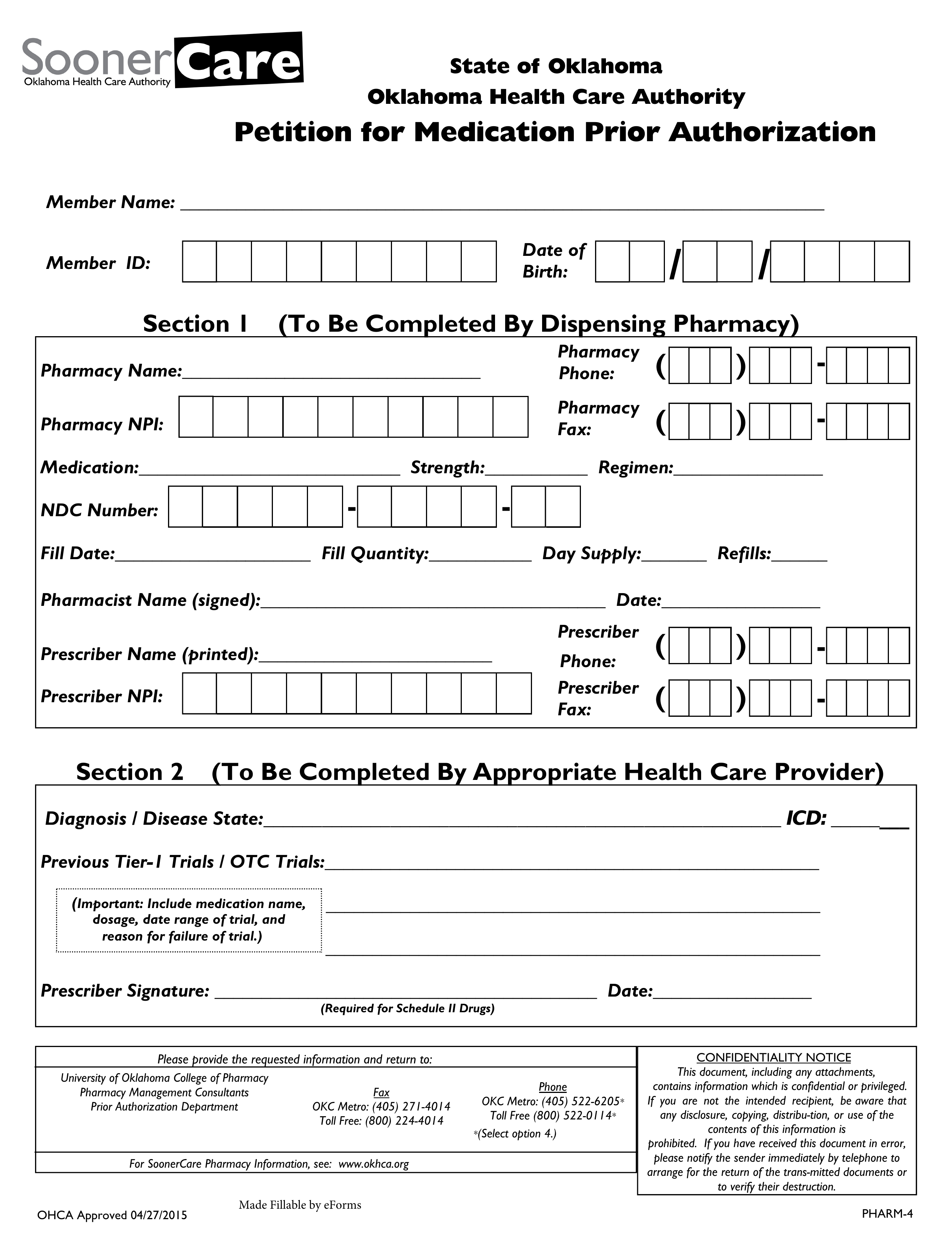
An Oklahoma Medicaid prior authorization form is a document employed by a medical office in order to request Medicaid coverage for a drug not on the State’s Preferred Drug List (PDL). We have provided a downloadable PDF version of this form on this webpage. Medicaid in the State of Oklahoma is provided by Soonercare, which is funded jointly by the federal and state government. If you require more information regarding Medicaid prior authorization, call the University of Oklahoma College of Pharmacy Pharmacy Management Consultants Prior Authorization Department at the phone number provided below.
Fax – 1 (800) 224-4014
Phone – 1 (800) 522-0114 (ext. 4)
Preferred Drug List (PDL)