Updated July 27, 2023
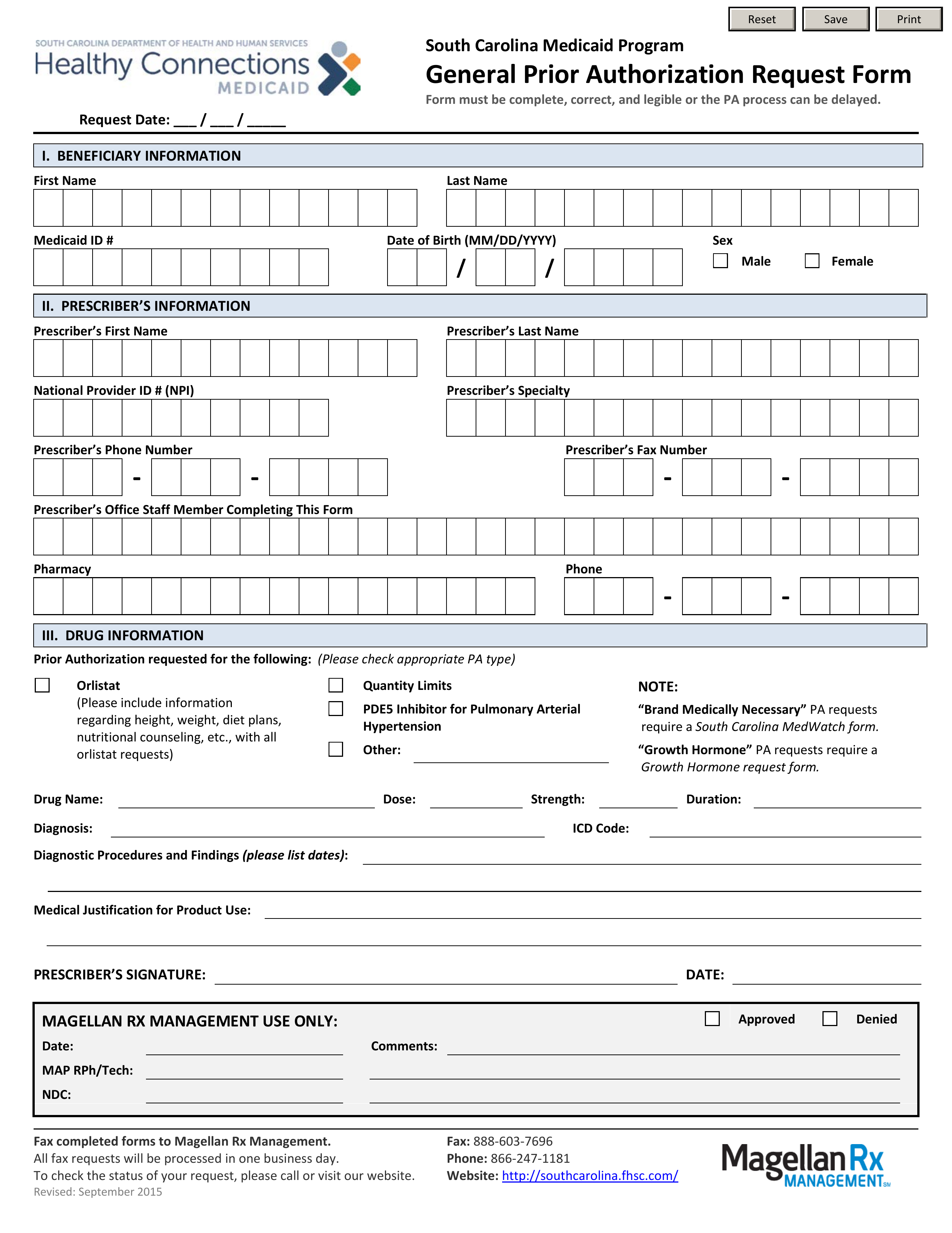
A South Carolina Medicaid prior authorization form is used by medical professionals who need to request Medicaid coverage for non-preferred therapies (not included on South Carolina Medicaid’s Preferred Drug List). The person making this request must provide clinical reasons for not prescribing a PDL drug. If you require further information, call the phone number provided below.
Fax – 1 (888) 603-7696
Phone – 1 (866) 247-1181
Preferred Drug List – Acceptable drugs by the State