Updated July 27, 2023
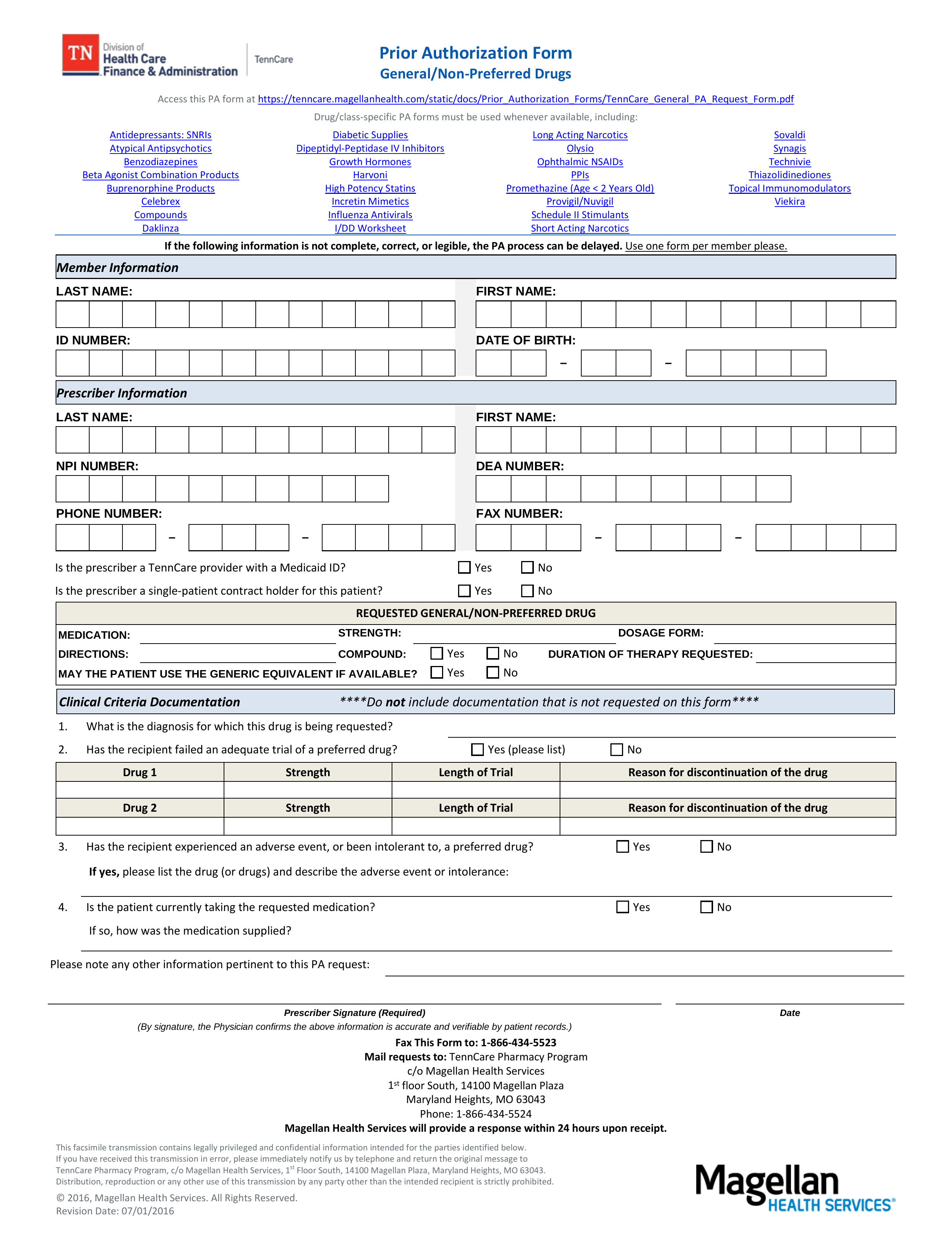
A Tennessee Medicaid Prior Authorization Form is a document used by medical offices in the State of Tennessee to request Medicaid coverage for a non-preferred drug. The person filling the form must provide medical justification as to why they are not prescribing a drug from the PDL (Preferred Drug List). Once the form has been completed, it should be submitted by fax or by mail to the directory indicated within the document.
Fax – 1 (866) 434-5523
Phone – 1 (866) 434-5524
Preferred Drug List (PDL)