Updated July 27, 2023
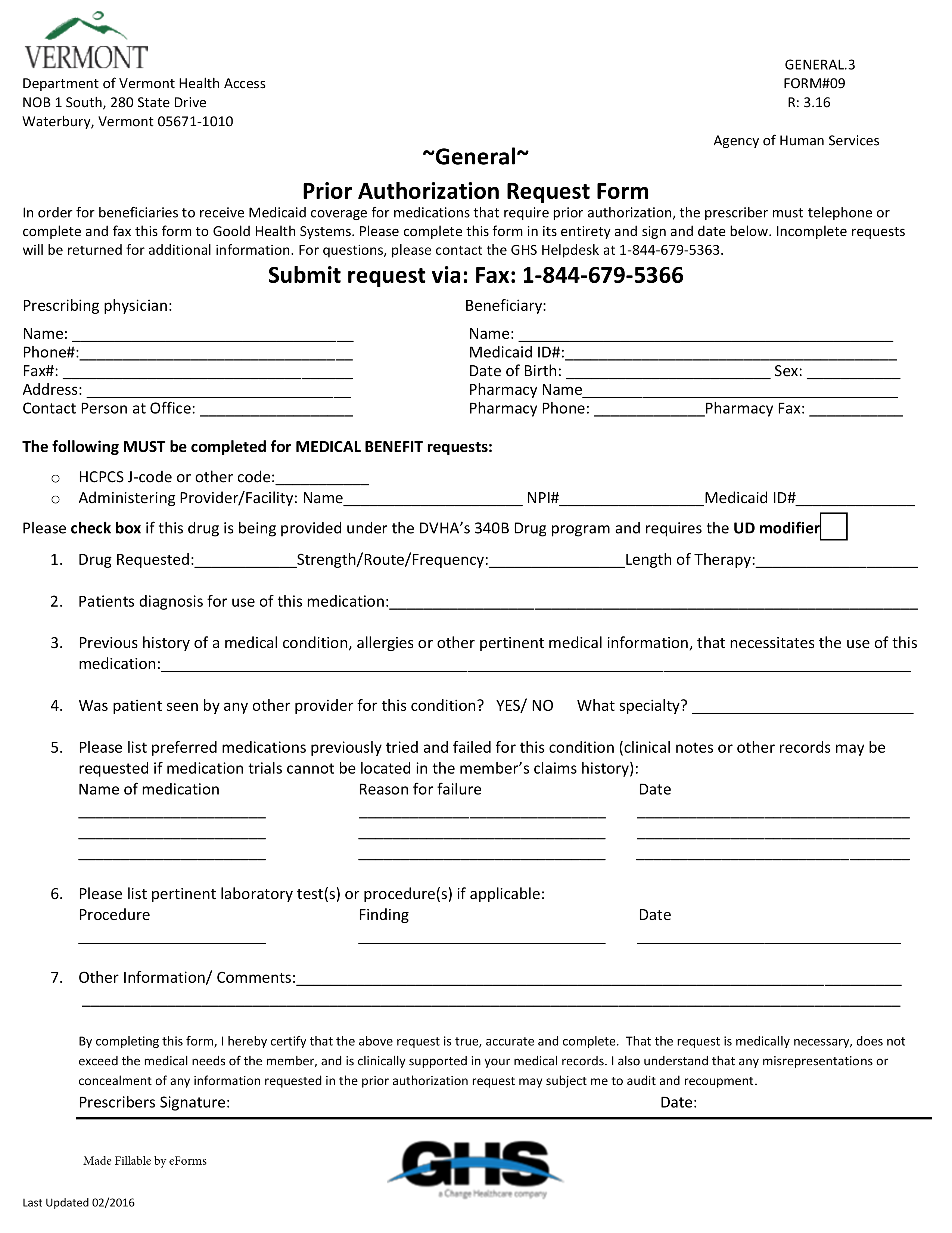
A Vermont Medicaid Prior Authorization Form is a document that is used to request Medicaid coverage for a non-preferred drug within the State of Vermont. In order for this request to be accepted, the prescriber must provide a proper medical justification for not prescribing a drug from the State-approved PDL (Preferred Drug List). On this page, you will find a downloadable PDF version of this form which can be either printed and filled out by hand, or filled out by computer using Adobe Acrobat or Microsoft Word. For more information, you can call the Goold Health Systems (GHS) Helpdesk at the phone number provided below.
Fax – 1 (844) 679-5366
Phone – 1 (844) 679-5363
Updated Preferred Drug List (PDL) – List of drugs pre-approved by the State