Updated July 27, 2023
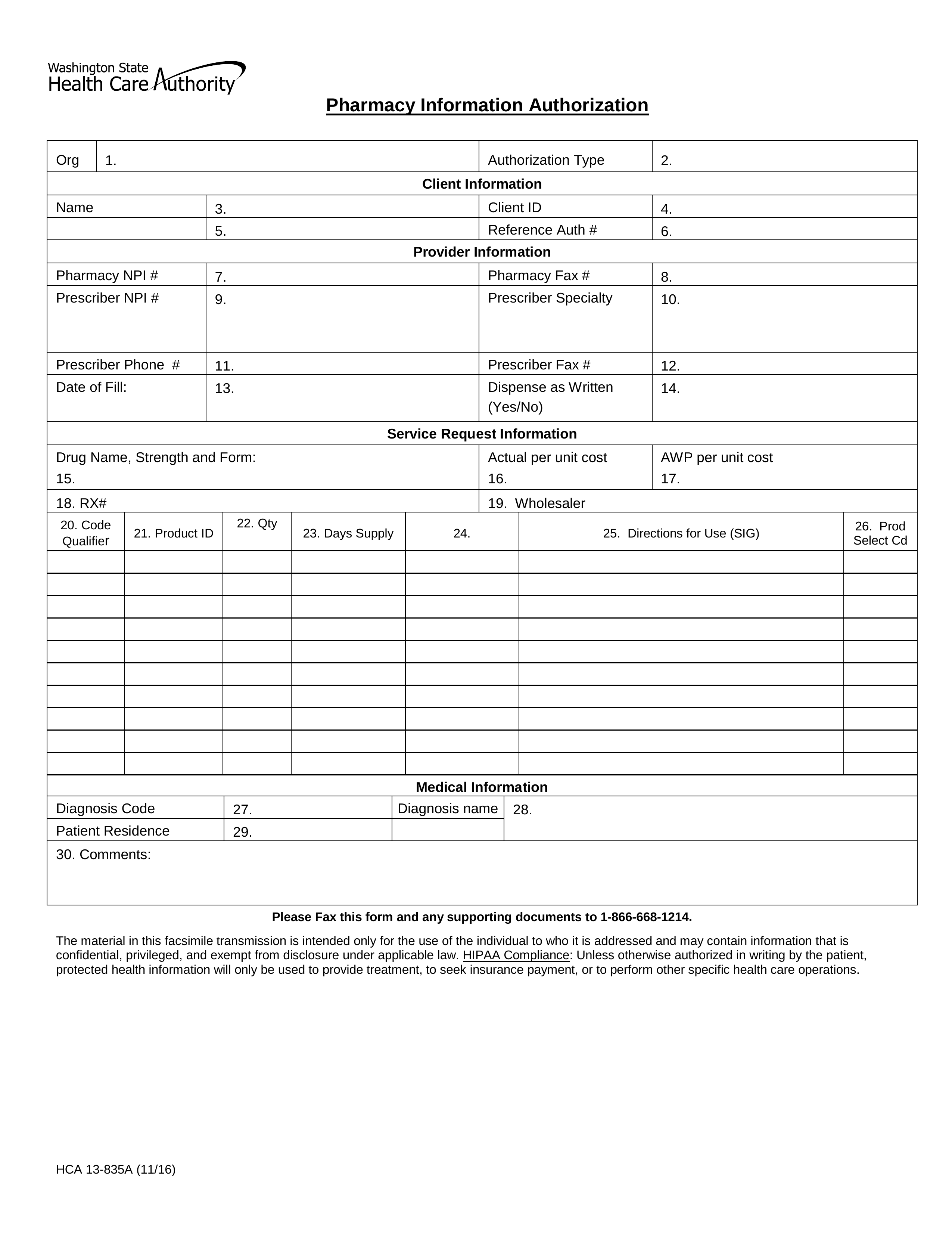
A Washington Medicaid prior authorization form is used by medical practitioners in Washington State when they need to request Medicaid coverage for a non-preferred medication. The reason for this process is that it encourages prescribers to favor prescribing drugs that appear on the State-approved Preferred Drug List (PDL). If you require more information, call the pharmacy authorization services line at the phone number provided below.
Fax – 1 (866) 668-1214
Phone – 1 (800) 562-3022 (ext. 15483)
Preferred Drug List (PDL)