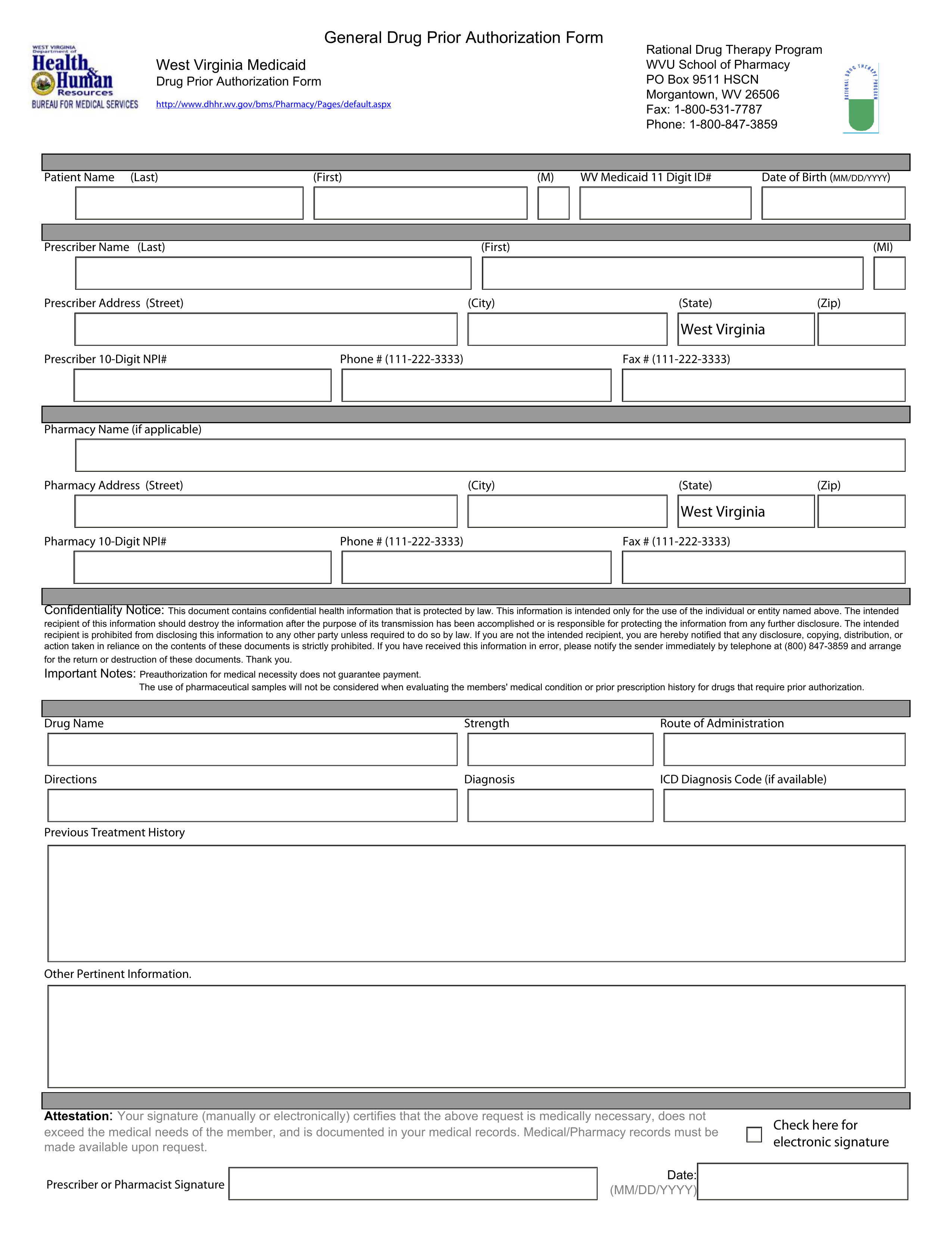
Updated July 27, 2023
A West Virginia Medicaid prior authorization form is completed and filed by a doctor who believes it’s medically necessary to prescribe a non-preferred drug to a patient. The physician has to justify their medical reasoning for prescribing a drug not included in the PDL. There is an established preferred drug list (PDL) that physicians must refer to when prescribing medication to their patients. The goal of the West Virginia Medicaid program is to make sure medications prescribed by registered providers are appropriate for the patient to whom the medication is being prescribed. The Drug Utilization Review Board makes the final decision on all prior authorization form submissions and even if the medical reasoning is sound, it’s possible that the request may be denied.
Form can be faxed to: 1 (800) 531-7787
Phone number: 1 (800) 847-3859