Updated July 27, 2023
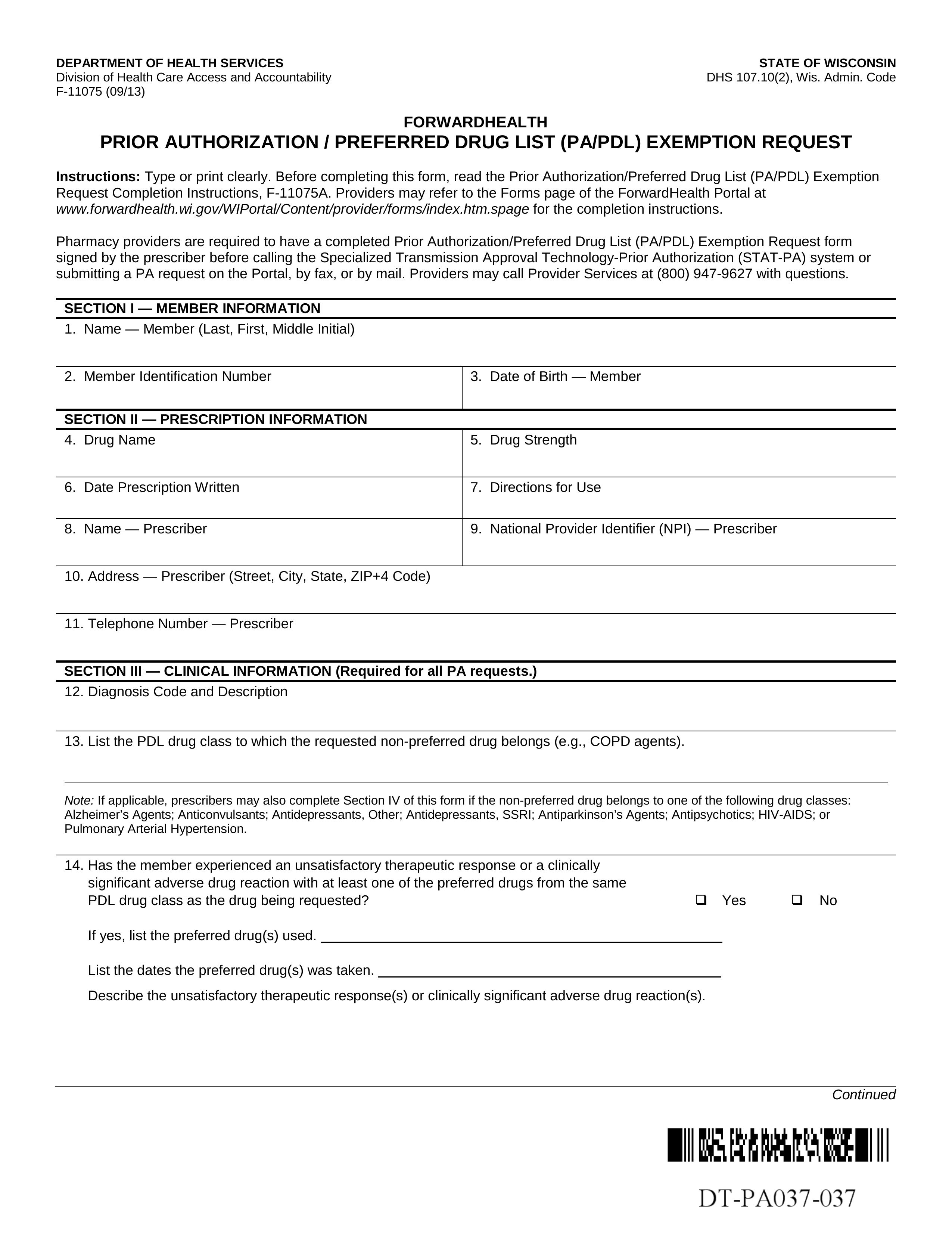
A Wisconsin Medicaid prior authorization form is a request form submitted by a physician who believes it is medically necessary to prescribe their patient a specific medication. Typically, Medicaid covers a wide range of prescriptions for their members but some medications must be put through a prior authorization procedure. The idea behind this is to make sure patients are receiving the most appropriate and cost-effective treatment available to avoid the misutilization of unnecessary medical services. The review board takes a number of variables into consideration such as provider certification, recipient eligibility, and medical necessity, before choosing to reimburse the prescription in question. We have provided the preferred drug list (PDL) below which includes all of the medications currently being covered by Wisconsin Medicaid.
Form can be faxed to: 1 (608) 221-8616
Phone number: 1 (800) 947-9627