Updated July 27, 2023
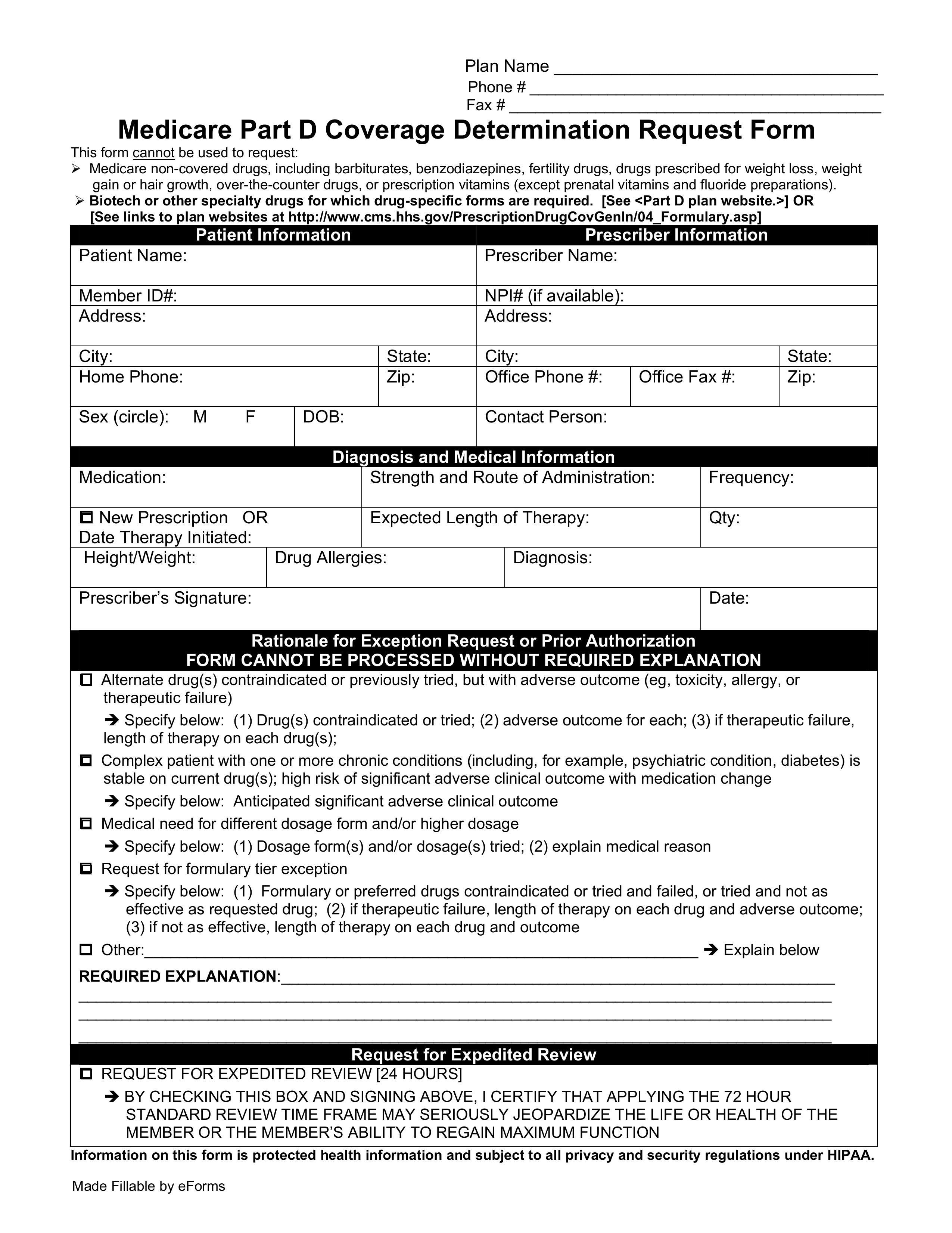
A Medicare prior authorization form, or drug determination request form, is used in situations where a patient’s prescription is denied at the pharmacy. Medicare members who have prescription drug coverage (Part D) will be covered for almost all their medication costs. Original Medicare members most likely have chosen to join a Medicare Prescription Drug Plan (PDP) for an additional premium. Members of Medicare Advantage (MA) Plans typically receive Part D coverage automatically; however, some plans require an additional monthly premium for drug coverage.
Once a patient, or their physician, receives a written denial (coverage determination), they should submit a coverage determination request form asking for the drug to be covered. The process is the same whether you receive your Part D coverage from a PDP or MA Plan. All plans must accept the standard coverage determination request form but some plans may have their own specific forms they prefer to use. The form must be mailed in or faxed directly to your plan’s office. Call your plan or check on their website to look up the proper mailing address or fax number.
Plans must respond within 72 hours of receiving your request form. If the physician feels the request is an emergency situation, an expedited review of 24 hours should take place. Once the request is approved, the medication will be usually be covered until the end of the calendar year.