Updated July 27, 2023
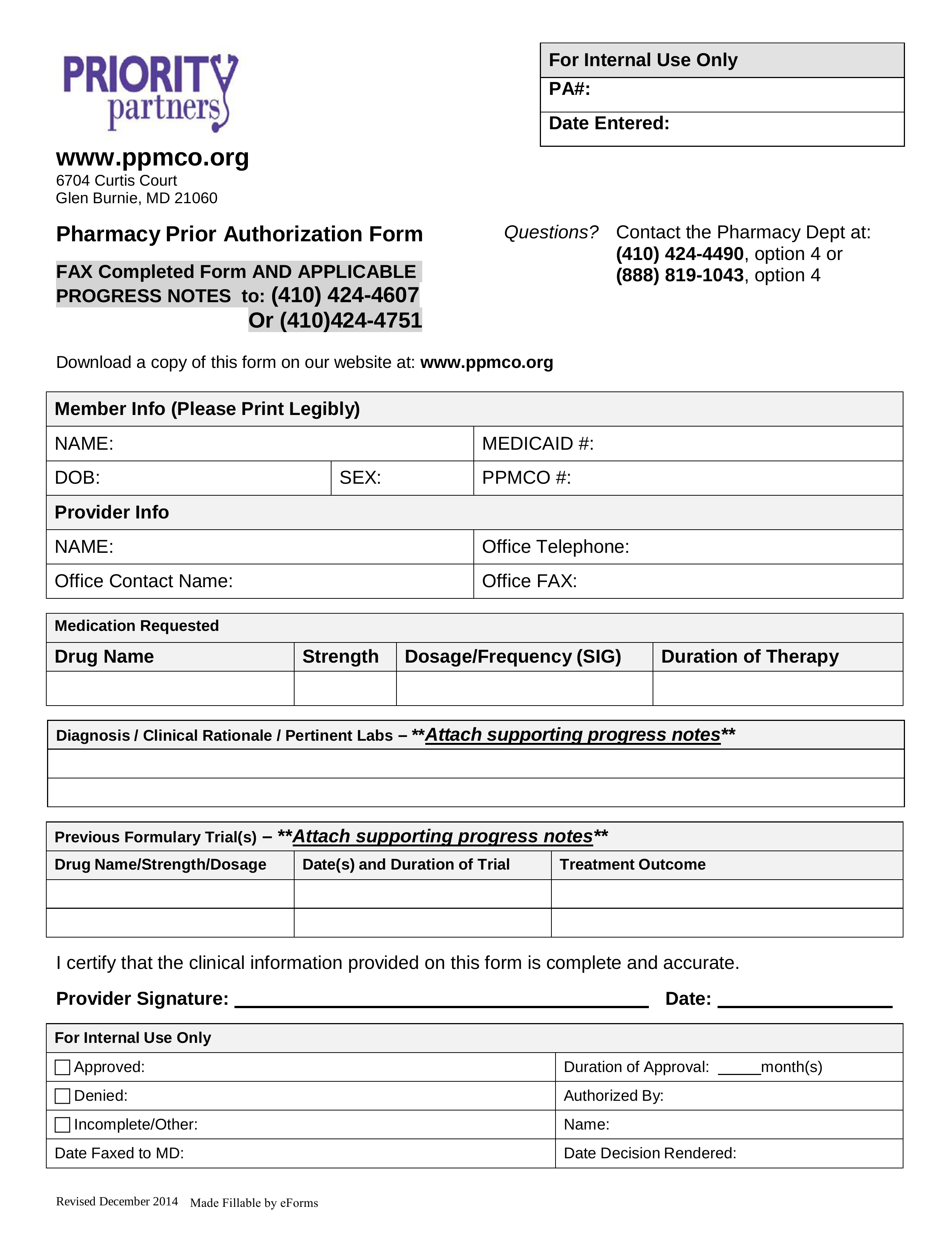
A Priority Partners prior authorization form allows a medical professional to request coverage for a medication that isn’t under the medical plan’s formulary. This is specifically for patients who are Priority Partners members through the John Hopkins Medicine LLC. The completed form can be submitted for review by sending it to one of the fax numbers provided below.
- Fax to: 1 (410) 424-4607 / 1 (410) 424-4751
- Phone: 1 (410) 424-4490 option 4 / 1 (888) 819-1043 option 4
- All Priority Partners Forms