Updated July 27, 2023
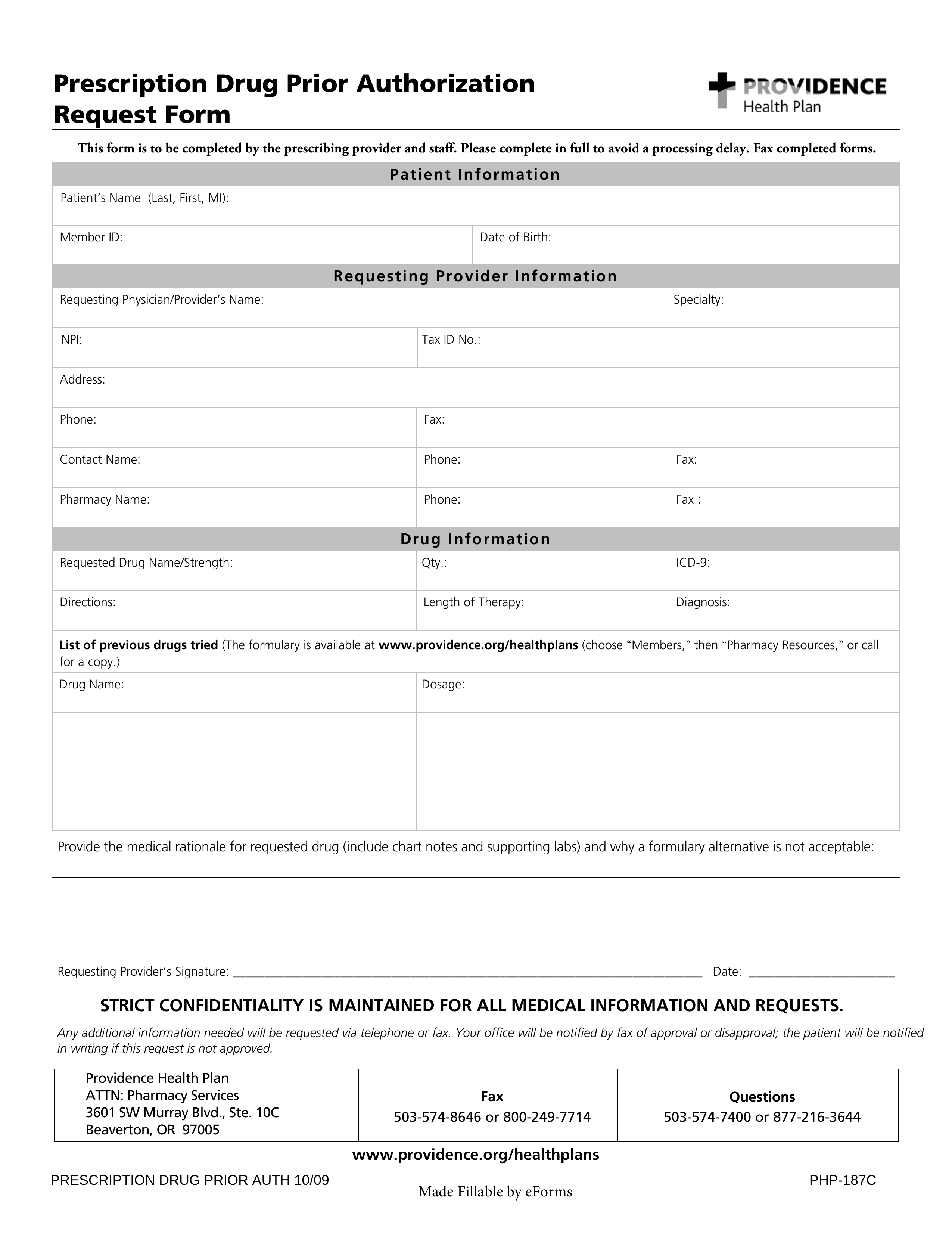
A Providence prior authorization form allows a physician to request coverage for a medication that their patient is not covered for with their Providence Health Plan. Within this form, they will need to justify their reasons for making this request and detail trials and tests which led to their diagnosis and resultant request. If you need to fill out a Providence prior authorization form for either medications or medical services, you can download fillable PDF versions of these forms on this page, and you will also find the fax numbers required for delivery purposes.
- Providence Prior Authorization Form
- Fax to: 1 (503) 574-8646 / 1 (800) 249-7714
- Phone: 1 (503) 574-7400 / 1 (877) 216-3644
- Providence Prior Authorization Form (Services Only)
- Services Requests Fax to: 1 (574)-6464 / 1 (800) 989-7479
- Services Requests Phone: 1 (574)-6400 / 1 (800) 638-0449