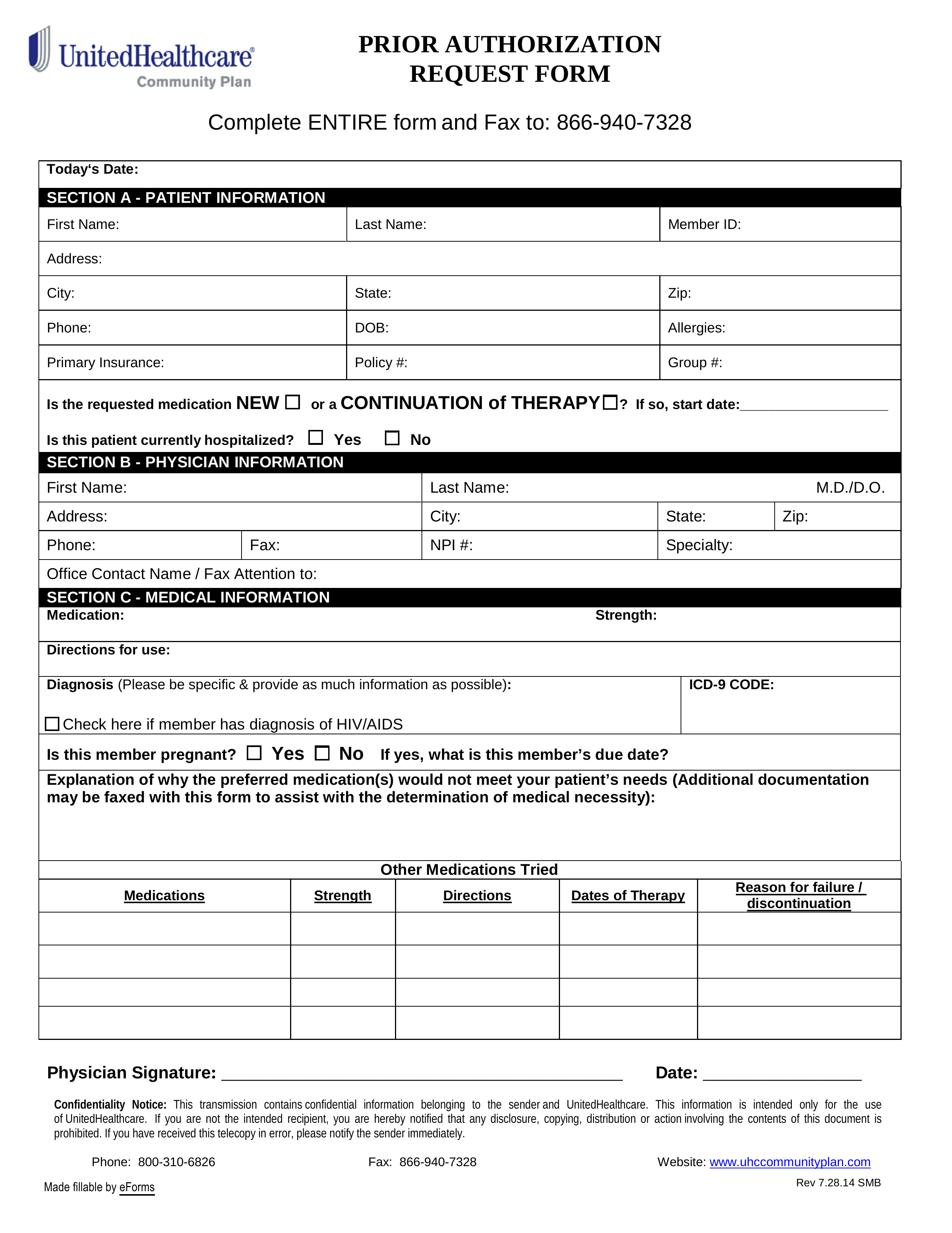
Updated July 27, 2023
A UnitedHealthcare prior authorization form is used by physicians in the instances they need to prescribe a medication that isn’t on the preferred drug list (PDL). Person’s covered under a UnitedHealthcare Community Plan (UHC) have access to a wide range of prescription medication. The purpose of this form is to demonstrate medical justification for prescribing the drug in question when other drugs on the PDL might serve the same purpose. The form should be submitted to UHC where they will review the physician’s medical reasoning and either approve or deny the prescription. If the request is denied, the patient may choose to pay for the drug out of pocket or ask the physician to prescribe a similar drug from the PDL.
Form can be faxed to: 1 (866) 940-7328
Phone number: 1 (800) 310-6826