Updated July 27, 2023
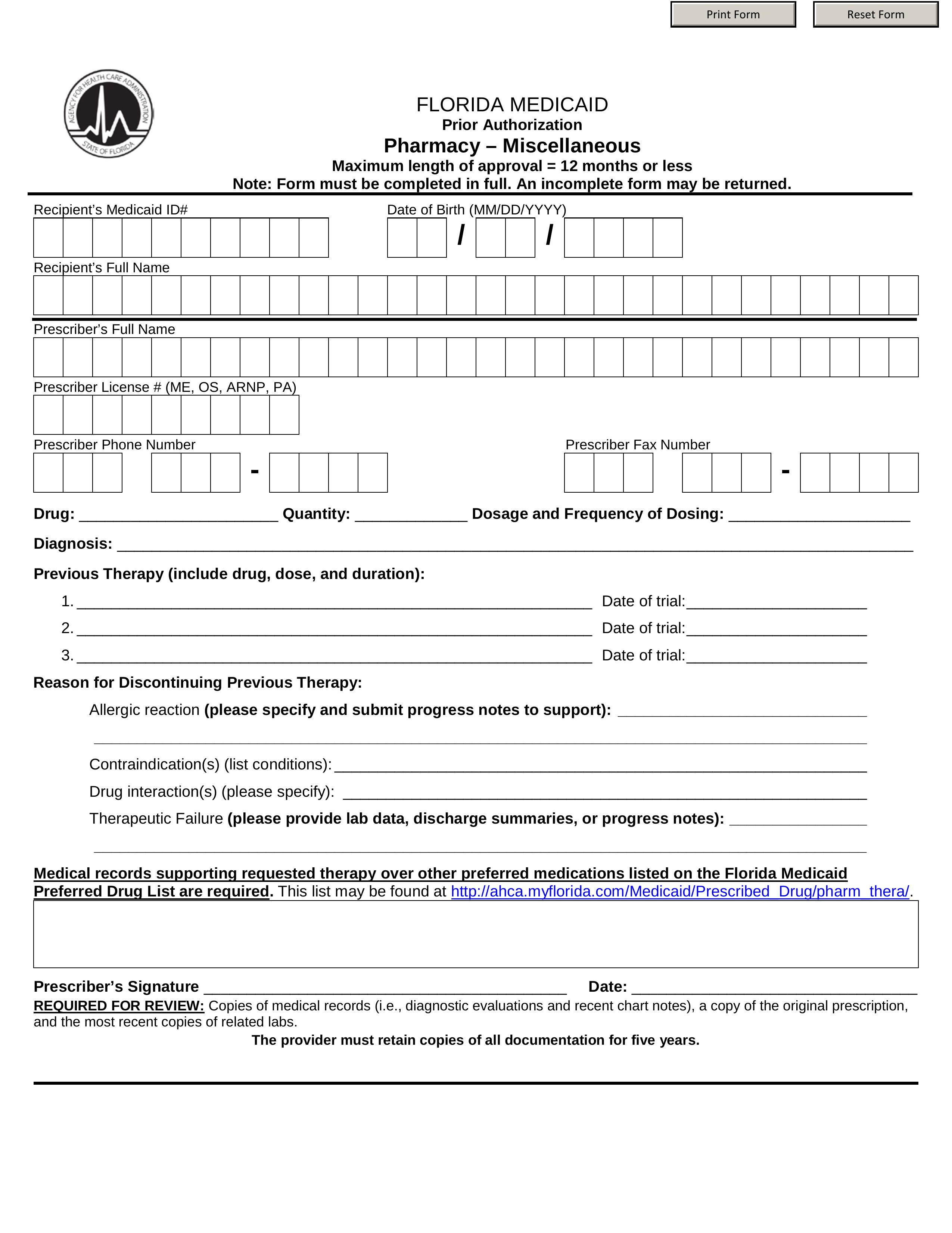
A Florida Medicaid prior authorization form is used by medical professionals to request State Medicaid coverage for a non-preferred drug prescription in the State of Florida. A non-preferred drug is one that is not on the State-approved Preferred Drug List (PDL). The physician must provide justification for their request, as well as attaching any relevant supporting documentation. Once completed, this form should be faxed or sent by mail to the correct directory.
Preferred Drug List – List of pre-approved drugs by the State