Updated July 27, 2023
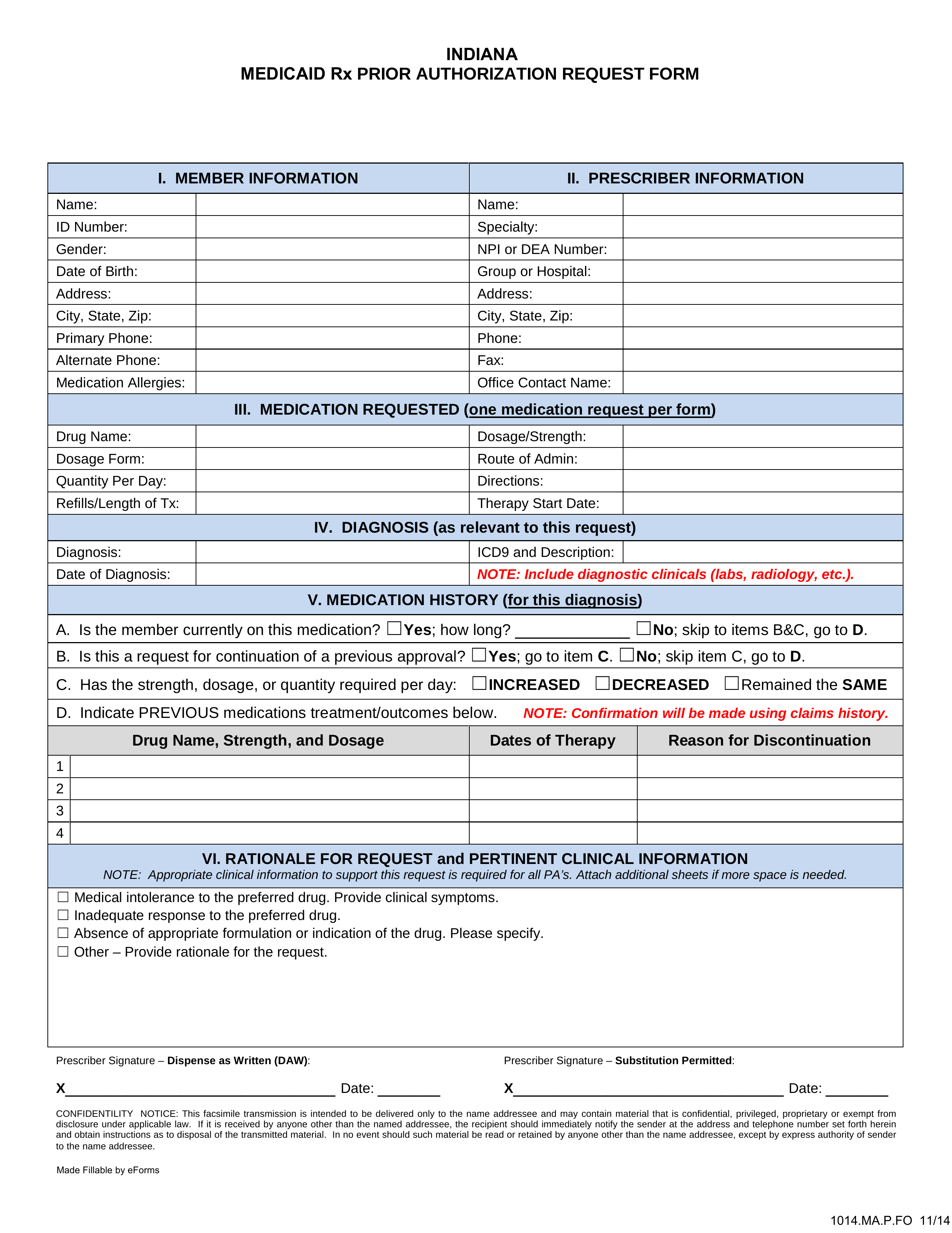
An Indiana Medicaid prior authorization form is a document used by medical professionals to request Medicaid coverage for a prescription drug not listed on the State’s preferred drug list. This form will provide the insurance company with the patient’s diagnosis, previous medications tried and failed, and any other information which could plead a case for the requested medication. Along with this form, you should submit any medical documentation which supports your justification for making this request.
Preferred Drug List – List of pre-approved drugs by the State