Updated July 27, 2023
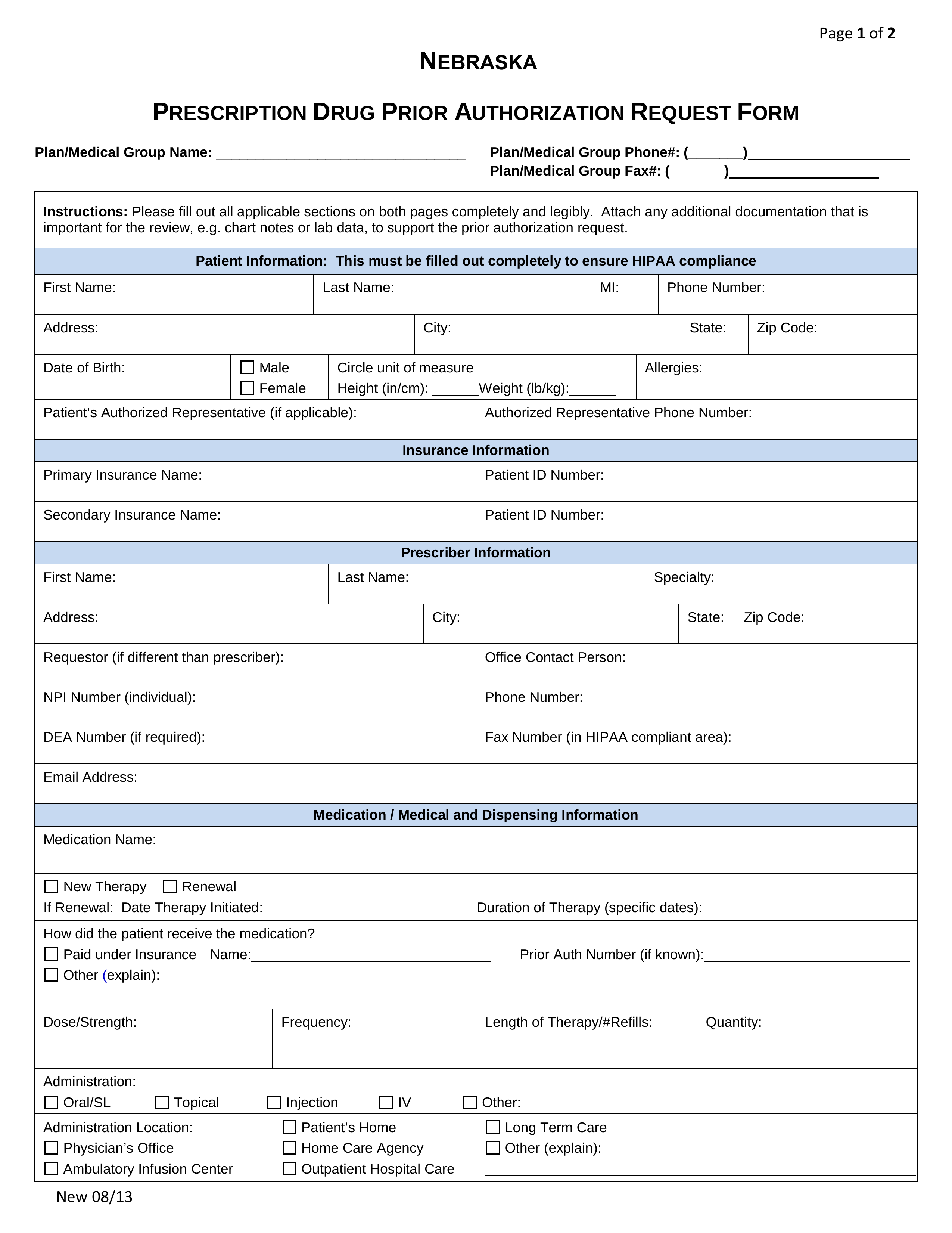
A Nebraska Medicaid prior authorization form allows a prescribing physician to request medications that are not covered by a patient’s Medicaid plan. This form is used to request a medication that is otherwise not on the preferred drug list (PDL). The physician must prove, with medical reasoning, that this particular drug is the best option for treating their patient’s condition. The form allows the physician to justify their diagnosis and provide clinical information to support their analysis. The Nebraska Medicaid prior authorization form must be signed by the prescribing physician and submitted to the Department of Health and Human Services for review.
- Form can be faxed to: 1 (866) 759-4115
- Phone number: 1 (800) 241-8335
- Preferred Drug List
- Other PA Forms