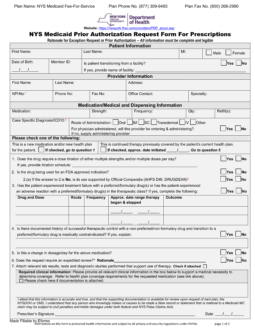
Updated July 27, 2023
A New York Medicaid prior authorization form is used when a medical practitioner needs to request Medicaid coverage for a drug that is not on the Preferred Drug List (PDL). In order for the request to be valid, the prescriber will need to present their medical justification(s) for not prescribing a preferred drug. Once completed, this form must be submitted via fax to the number provided below. A fillable PDF version is of the form is available on this page (compatible with Adobe Acrobat and Microsoft Word).
Fax – 1 (800) 268-2990
Phone – 1 (877) 309-9493
Preferred Drug List – Drugs deemed acceptable for prescription by the State