Updated July 27, 2023
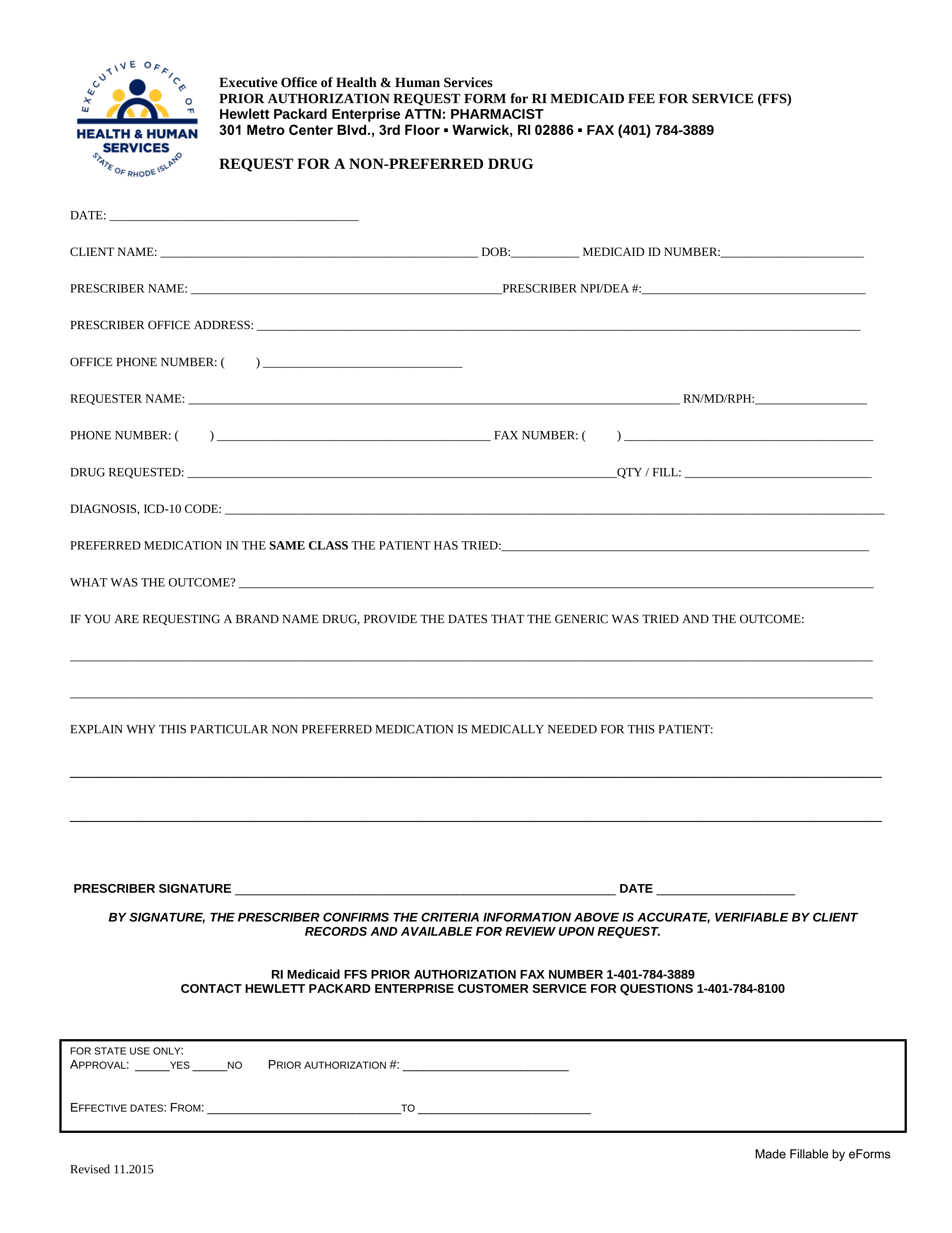
A Rhode Island Medicaid prior authorization form requests Medicaid coverage for a non-preferred drug. Once completed, this form must be submitted by fax to the number found immediately below this paragraph, or by mail to the address found within the document. For more information, call the Rhode Island Department of Human Services’ Medicaid department at the phone number provided below.
Fax – 1 (401) 784-3889
Phone – 1 (401) 462-5300
Preferred Drug List – Acceptable drugs by the State