Updated July 31, 2023
A surgical consent form is used to ensure a patient has been provided with all the necessary information concerning a proposed surgery/special procedure and to document that they agree to undergo the operation. Any risks associated with the procedure and treatment thereafter must be outlined in the form. Even with minor, non-life-threatening surgeries, there should be no guarantees, either implicit or explicit. A separate section on anesthesia is included in the consent form as the risks are different than those involved with the actual surgery/procedure. If a blood transfusion is necessary, the patient’s doctor should also inform them of the risks and benefits associated with this process. The patient must sign the surgical consent form once they have an understanding of the whole procedure. If they are unable to sign, a legal representative must sign the document.
How to Write
Step 1 – Download in PDF, Microsoft Word, or Open Document Text.
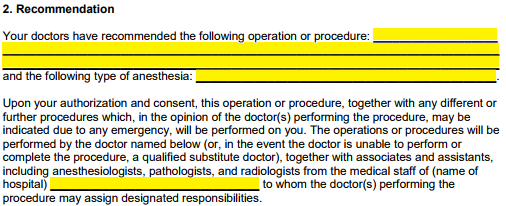
Step 2 – The operations recommended by the doctors should be listed under the “Recommendation” section of the consent form, along with the types of anesthesia to be administered. Next, the hospital’s name where the surgery is to take place should be entered in the available space.
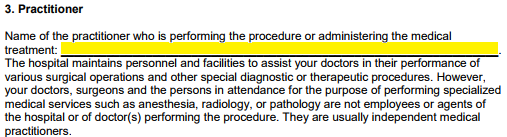
Step 3 – The surgeon’s name must be indicated in the field provided under the “Practitioner” section.
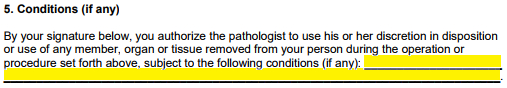
Step 4 – Section 5 informs the patient that the pathologist may dispose of or use any member, organ, or tissue removed during the operation. If any conditions apply, they may be entered in the empty field provided.
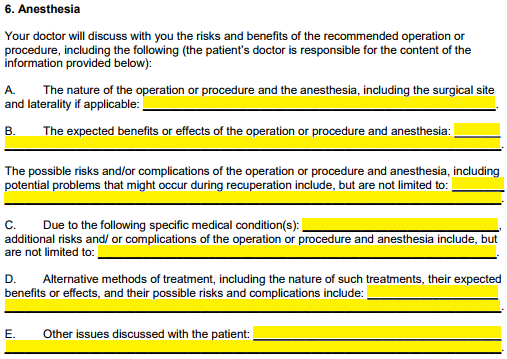
Step 5 – Under Section 6, “Anesthesia,” information regarding the surgery/procedure, the anesthesia involved, possible risks/effects, and treatments administered post-surgery can be entered in the appropriate spaces provided under Parts “A” through “E.”
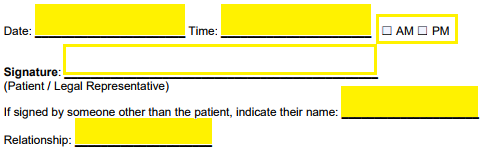
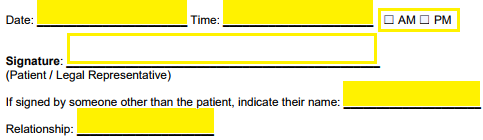
Step 6 – The patient must sign page 3, as shown below, with the current date. If a legal representative has signed, due to the patient being incapacitated somehow, they must print their name and enter their relationship with the patient.
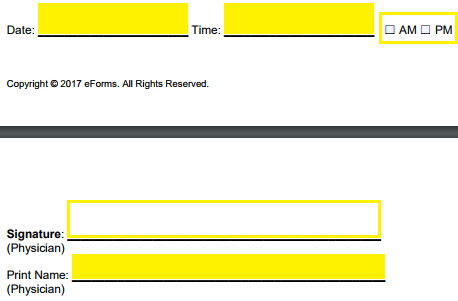
Step 7 – Next, the physician must sign the form under the “Physician Certification” section and include the date and their printed name.
Step 8 – Under the “Consent to Blood Transfusion” section, any special instructions for the patient’s blood transfusion should be mentioned in the blank fields.
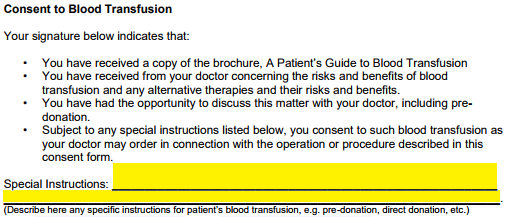
Step 9 – The patient must provide their signature once more under the “Consent to Blood Transfusion” section, along with the date. Or, if the patient cannot sign, a legal representative must do so and include their printed name and relationship to the patient.
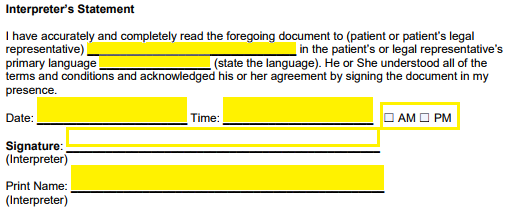
Step 10 – If it was necessary for the patient to have an interpreter present during the explanation of the surgery/procedure and the risks involved, the interpreter must sign, date, and print their name after entering the name of the patient and their native language.