Updated July 27, 2023
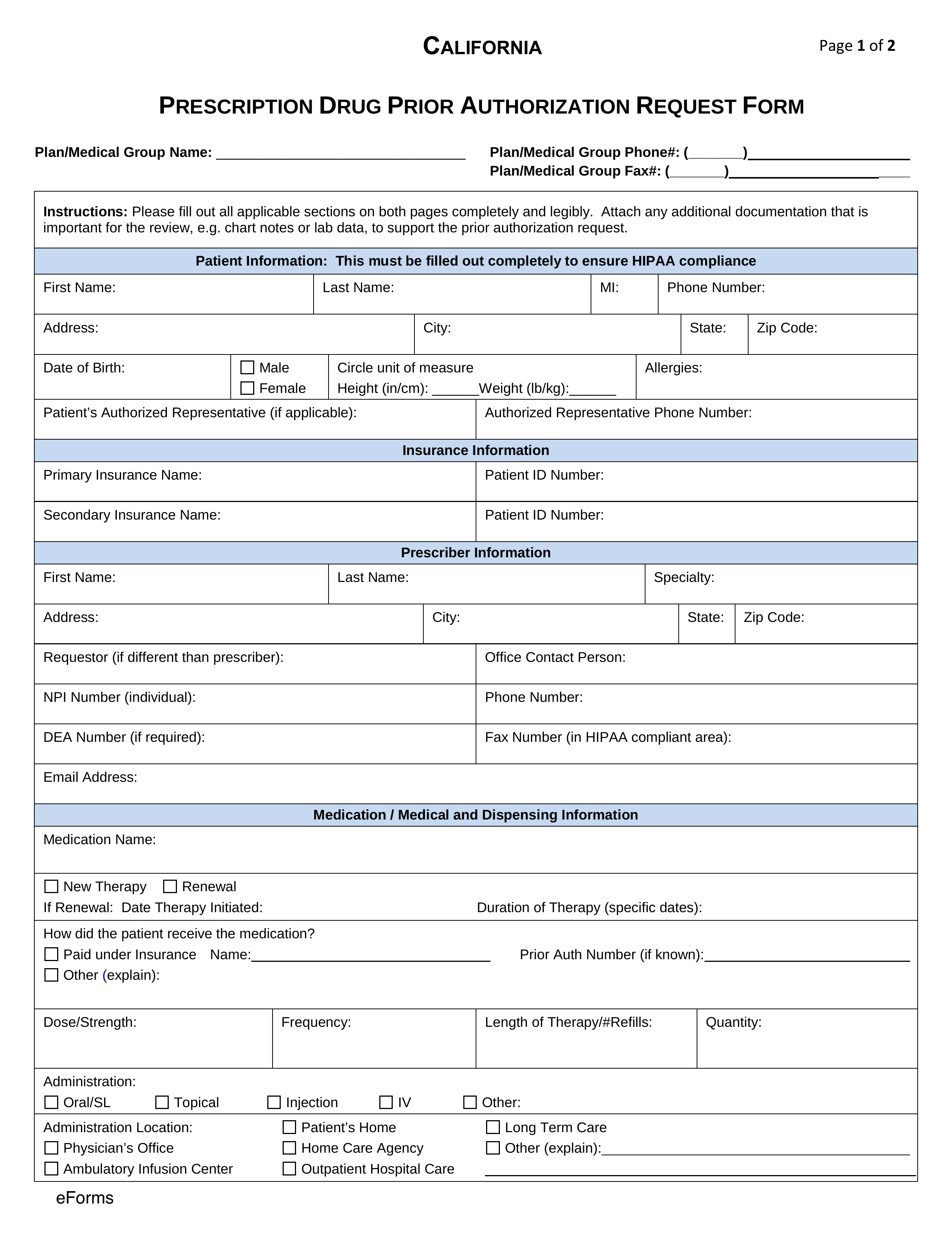
A California Medicaid prior authorization form is a request document that must be completed by a physician prescribing a drug for a patient using Medi-Cal that is not on the state’s Preferred Drug List (PDL). Medi-Cal pharmacy benefits cover most prescription medications but, if a doctor deems it medically necessary to prescribe medication not on the PDL, they must justify their diagnosis in the prior authorization form. The reviewing process could take quite a few days and just because a physician provides solid medical reasoning does not mean the request will be approved. Patients will be informed of their options should the prior authorization request be denied.
Note that the contact information differs depending on the type of California Medicaid prior authorization form request.
- Self-administered non-specialty medications (US Script)
- Fax number:1 (866) 399-0929
- Phone number: 1 (877) 277-0413
- Self-administered specialty medications (AcariaHealth)
- Fax number: 1 (855) 217-0926
- Phone number: 1 (855) 535-1815
- Physician-administered specialty medications (California Health & Wellness Pharmacy Department)
- Fax number: 1 (877) 259-6961
- Phone number: 1 (877) 658-0305