Updated July 27, 2023
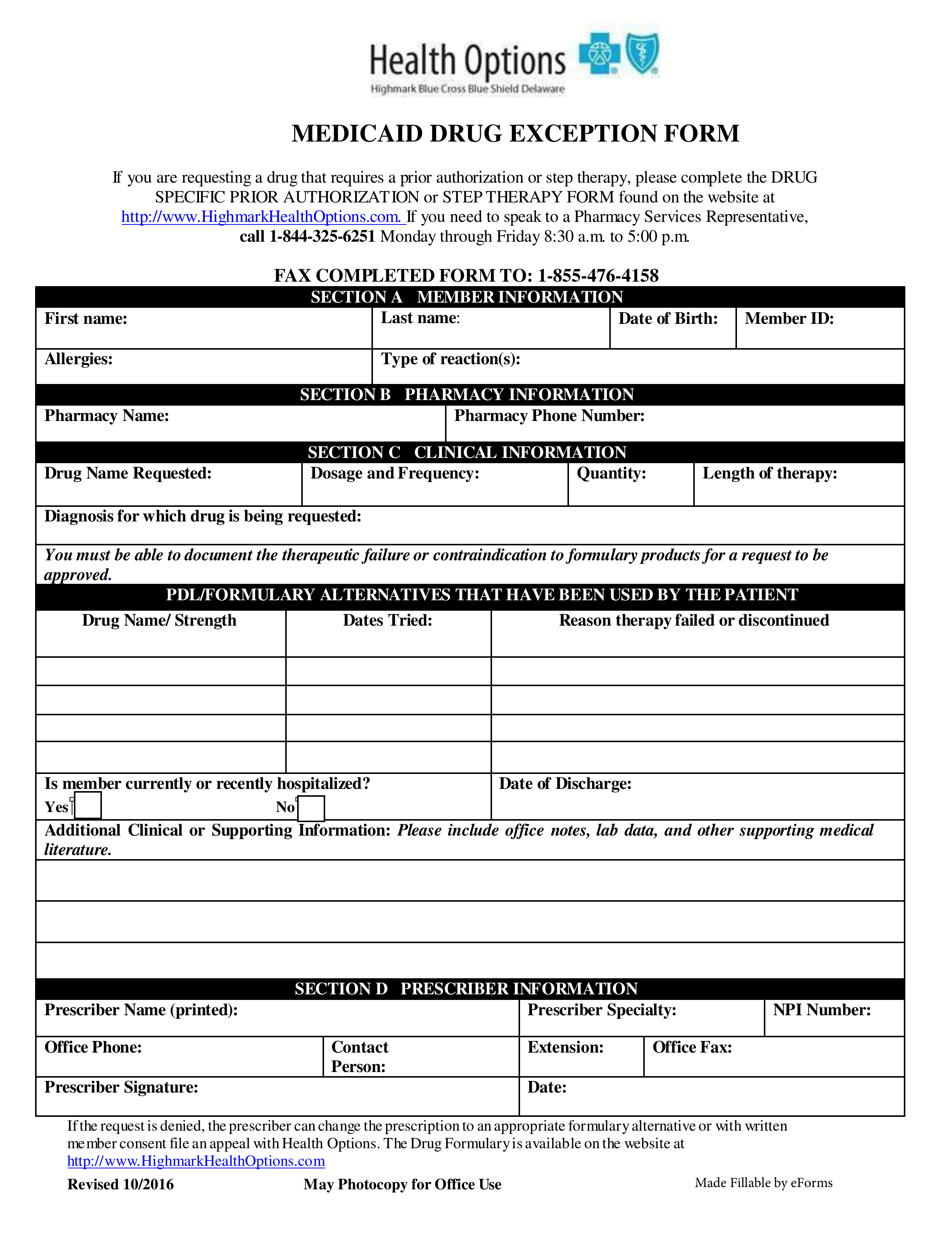
A Delaware Medicaid prior authorization form is used by healthcare providers wishing to request Medicaid coverage for a patient’s prescription. When making a prior authorization request, the physician must provide supporting documentation and a written justification for requesting coverage of the specific medication in question. Call the number below if you require more information.
DMMA Provider Relations Phone # – 1 (800) 999-3371
Delaware Medical Assistance Portal (DMAP)
DMAP Preferred Drug List – List of pre-approved drugs by the State