Updated July 27, 2023
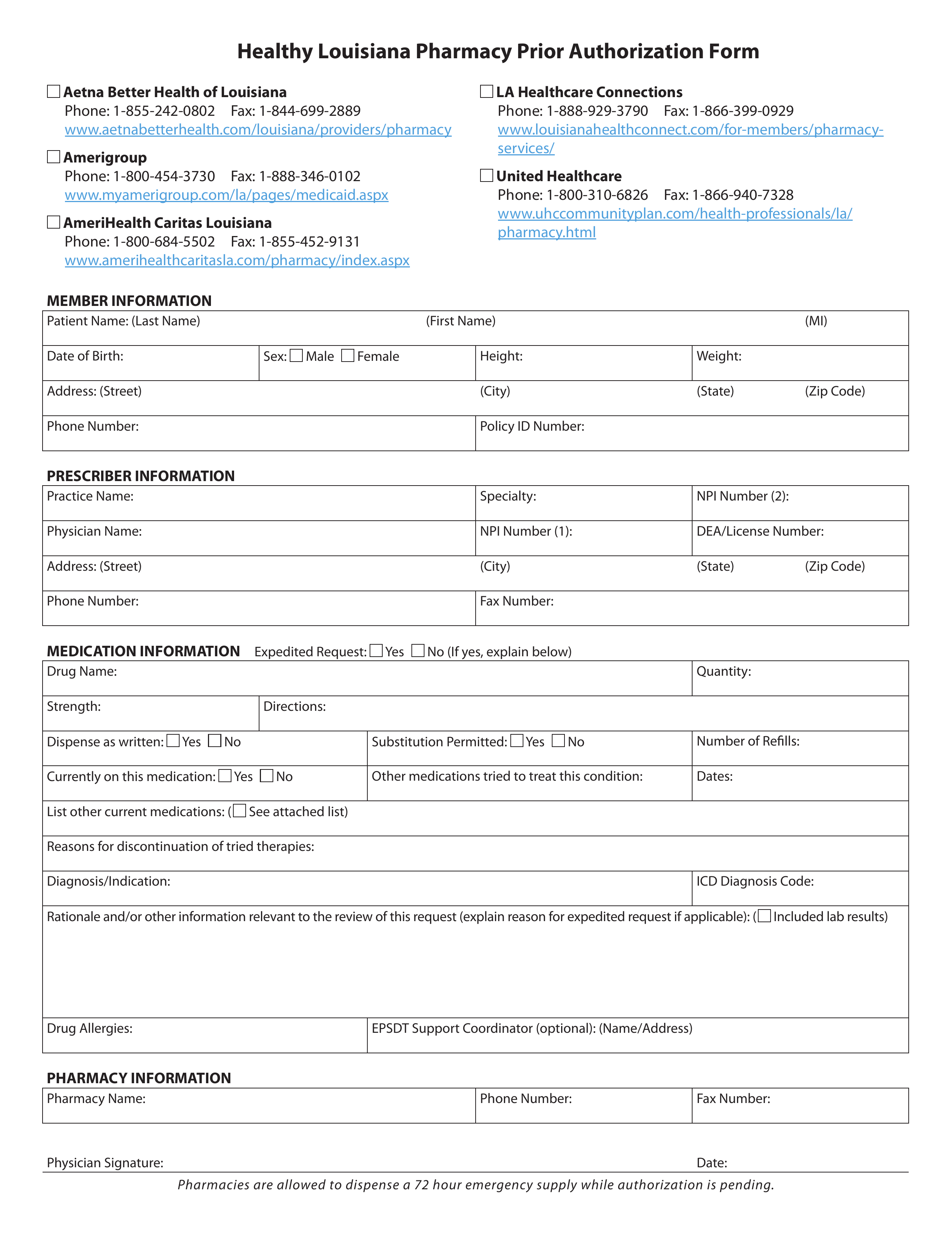
A Louisiana Medicaid prior authorization form is used when a medical professional wishes to request coverage for a prescription that is not normally covered by Medicaid because is not on the Preferred Drug List (PDL). In the State of Louisiana, Medicaid is handled by Healthy Louisiana, the department of health’s program to expand healthcare coverage for low-income individuals. On this webpage, you can download a PDF version of this form and fill it out by using either Adobe Acrobat or Microsoft Word. For more information on prior authorization or to make a prior authorization request by phone, call the number provided immediately below this paragraph.
Phone – 1 (800) 488-6334
Preferred Drug List (PDL) – List of pre-approved drugs by the State